R52.9
DESCRIPTION
Cancer pain is usually persistent and progressive. Pain assessment requires training in:
- psycho-social assessment
- assessment of need of type and dose of analgesics
- pain severity assessment
Pain severity and not the presence of pain determine the need for treatment.
Medicinal treatment for pain should never be withheld.
Pain is what the patient says it is.
Under-recognition of pain and under-dosing with analgesics is common in chronic cancer pain.
Analgesics should be given regularly rather than only when required in patients with ongoing pain.
GENERAL MEASURES
- Counselling/hospice care.
- Occupational therapy may be required.
- Management of psycho-social factors.
Note:
- Appropriate care is provided from the time of diagnosis.
- Home palliative care is provided by the family or caregiver with the support of health care professionals. See: Medicines used in palliative care.
MEDICINE TREATMENT
Pain should be controlled as rapidly as possible. If pain is not adequately controlled within 2 days, proceed to the next step. Cancer pain in children is managed by the same principles but using lower doses of morphine than adults.
RECOMMENDED STEPS IN MANAGEMENT OF CANCER PAIN
Adults
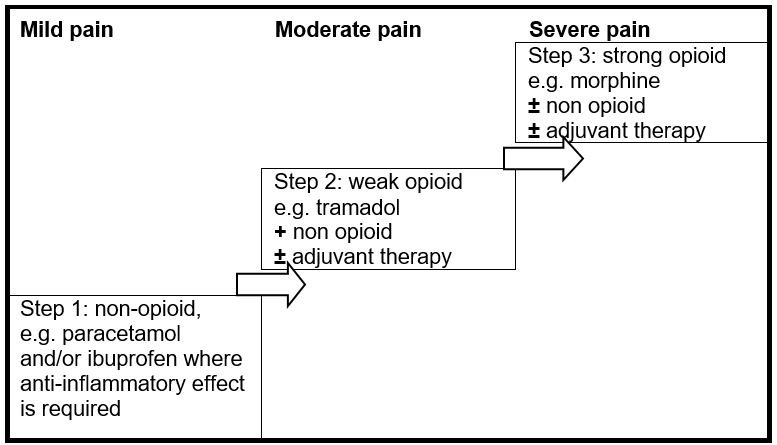
Step 1
Non-opioid
- Paracetamol, oral, 1 g 4–6 hourly when required.
- Maximum dose: 15 mg/kg/dose.
- Maximum dose: 4 g in 24 hours.
AND/OR
- NSAIDs, e.g.:
- Ibuprofen, oral, 400 mg 8 hourly with or after a meal.
Step 2
Add weak opioid to Step 1
- Tramadol, oral, 50 mg, 4–6 hourly as a starting dose (Doctor prescribed).
- May be increased to a maximum of 400 mg daily.
CAUTION
Use with caution when administered with antidepressants e.g. amitryptyline to avoid over sedation.
Step 3
Paracetamol and/or ibuprofen can be used with morphine in step 3
- Morphine, oral, 4 hourly (Doctor prescribed).
- Start with 5–10 mg.
- Titrate the dose and dose frequency against the effect on pain.
If dosage is established and patient is able to swallow:
- Morphine, long-acting, oral], 8–12 hourly (Doctor prescribed).
- Start with 10–20 mg/dose.
- Titrate the dose and dose frequency against the effect on pain
Elderly adults or severe liver impairment:
- Morphine solution, oral, 4 hourly. (Doctor prescribed).
- Start with 2.5–5 mg.
- Titrate the dose and dose frequency against the effect on pain.
Titrate the dose and dose frequency against the effect on pain
Note:
- There is no maximum dose for morphine – dose is titrated upward against the effect on pain.
- For the management of morphine overdose, see Exposure to poisonous substances
Children
Stepwise approach to pain management is recommended:
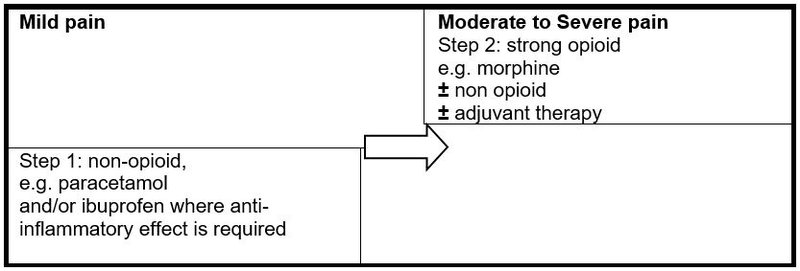
Non-opioid
- Paracetamol, oral, 10–15 mg/kg/dose 6 hourly when required See paediatric dosing tool.
- NSAIDs, e.g.:
- Ibuprofen, oral, 5–10 mg/kg/dose 8 hourly with or after a meal. See paediatric dosing tool.
- Where anti-inflammatory effect is required.
- Can be used in combination with paracetamol or opioids.
- Discontinue if not effective after 2–3 days.
Opioid
- Morphine, oral, 0.2–0.4 mg/kg/dose 4–6 hourly according to severity of the pain. See paediatric dosing tool. (Doctor prescribed).
Adjuvant therapy:
Adults
In addition to analgesia as above:
- Amitriptyline, oral, 25 mg at night. (Doctor initiated).
- Titrate up to a maximum of 75 mg at night.
Significant nausea and vomiting:
Adults
- Metoclopramide oral, 10 mg, 8 hourly as needed.
Children
For treatment of nausea and vomiting in the palliative care setting, see Nausea and vomiting.
Constipation:
A common problem due to long-term use of opioids, which can be prevented and should always be treated.
Children
- Lactulose, oral, 0.5 mL/kg/dose once daily. See paediatric dosing tool.
- If poor response, increase frequency to 12 hourly.
Adult
- Lactulose oral, 10–20 mL once daily.
- If poor response, increase frequency to 12 hourly.
(See: Constipation for further management of palliative constipation).
For pruritus:
Children
- Chlorphenamine, oral, 0.1 mg/kg/dose 6–8 hourly. See paediatric dosing tool.
Adults
- Chlorphenamine, oral, 4 mg, 6–8 hourly.
CAUTION
Do not give an antihistamine to children < 2 years of age.
For anxiety:
Children
- Diazepam, oral, 0.04 mg/kg/dose 8–12 hourly (Doctor prescribed).
|
Weight kg |
Dose mg |
Tablet 2 mg |
Age months/years |
|---|---|---|---|
| > 9 - 17.5 kg | 0.5 mg | ¼ tablet | > 12 mths - 3 yrs |
| > 17.5 - 25 kg | 1 mg | ½ tablet | > 5 - 7 yrs |
| > 25 - 35 kg | 1.5 mg | ¾ tablet | > 7 - 11 years |
| > 35 kg | 2mg | 1 tablet | > 11 yrs |
- May be increased to 0.2 mg/kg/dose 8–12 hourly.
- Beware of respiratory depression if given with morphine.
- Diazepam, oral, 0.2 mg/kg/dose 8–12 hourly (Doctor prescribed)
- Beware of respiratory depression if given with morphine.
|
Weight kg |
Dose mg |
Use one of the following tablets: |
Age months/years |
|
|---|---|---|---|---|
| 2 mg | 5 mg | |||
| > 9 - 11 kg | 2 mg | 1 tablet | > 12 - 18 mths | |
| > 11 - 14 kg | 2.5 mg | ½ tablet | > 18 mths - 3 yrs | |
| > 14 - 17.5 kg | 3 mg | 1½ tablets | > 5 - 7 yrs | |
| > 17.5 - 25 kg | 4 mg | 2 tablets | > 5 - 7 yrs | |
| > 25 kg | 5 mg | 1 tablet | > 7 years |
Adults
- Diazepam, oral, 2–5 mg every 12 hours for a maximum of two weeks. (Doctor prescribed)
Breakthrough pain:
Breakthrough pain is pain that occurs before the next regular dose of analgesics. This is due to an inadequate regular dose.
It is recommended that an additional dose of morphine (up to the same dose as the regular 4-hourly dose) be administered for breakthrough pain. The next regular dose of morphine must still be given at the prescribed time, and not be delayed because of the additional dose.
The regular 4-hourly dosage should be titrated upward against the effect on pain in the following way:
- Add up the amount of “breakthrough morphine” needed in 24 hours.
- Divide this amount by 6 (the number of 4 hourly doses in 24 hours).
- The next day increase each dose by that amount.
Example:
Patient gets 10 mg morphine every four hours.
The patient has 3 episodes of breakthrough pain:
3 x 10 mg = 30 mg
30 mg ÷ 6 = 5 mg
The regular 4 hourly dose of 10 mg will be increased by 5 mg
i.e. 10 mg + 5 mg = 15 mg.
The increased morphine dose will be 15 mg 4 hourly.
REFERRAL
- Uncontrolled pain.
- Pain uncontrolled by step 1 if no doctor available.
- Severe emotional or other distress which may aggravate the perception of pain.
- Nausea and vomiting associated with pain in children.