P29.8
Be prepared
Be at the delivery
Check the equipment and emergency medicines
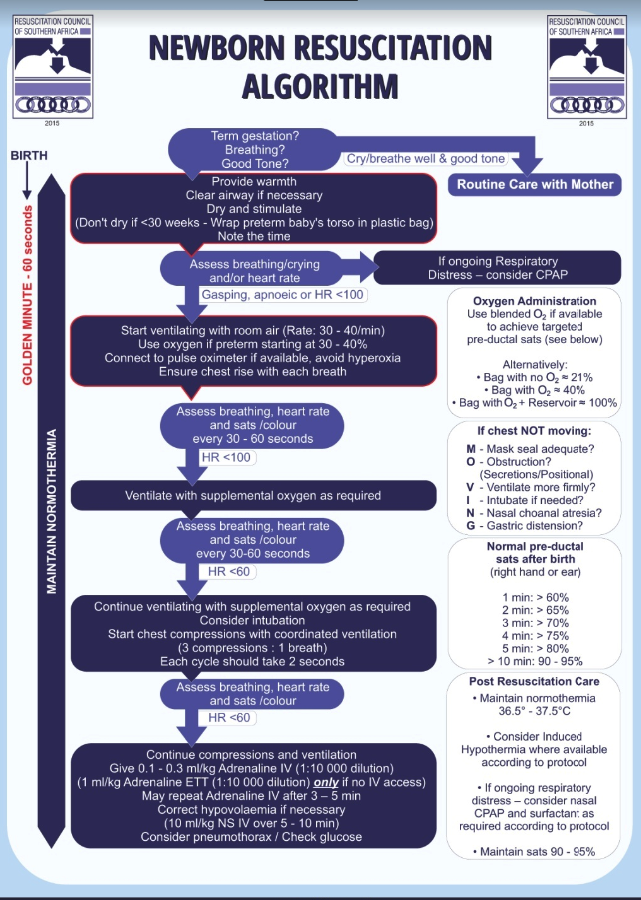
- Follow the algorithm at the end of the section.
- Check that each step has been effectively applied before proceeding to the next step. The algorithm follows the assumption that the previous step was unsuccessful and the baby is deteriorating.
- Use oxygen concentration that alleviates central cyanosis, obtains target pulse oximetry readings (if pulse oximeter is available), and restores a heart rate >100 beats/minute. Bag and mask ventilation should be initially done with room air. (There is evidence that routine resuscitation with 100% oxygen is potentially harmful to the baby).
An unsatisfactory response to resuscitation includes:
- A sustained slow heart rate, usually ≤ 60 beats/minute or a progressive decrease in heart rate until cardiac arrest occurs.
- Episodes of cardiac arrest, with a progressively weaker response to chest compressions, positive pressure ventilation and medicines.
- A decreasing blood pressure, increasing acidosis, severe hypotonia with central cyanosis or intense pallor.
- Apnoea or weak, irregular and inefficient respiratory efforts.
MEDICINE TREATMENT
If baby’s response to resuscitation is inadequate once ventilation and circulation are adequately supported the following steps should be carried out:
If the mother is known or suspected to have had narcotic pain relief and the baby has normal heart rate and colour response to bag-mask ventilation, but has not initiated sustained regular respiratory effort:
- Naloxone, IV, 0.1 mg/kg.
Check the blood glucose of the baby.
If hypoglycaemia is present: E16.0-2
- Dextrose 10%, IV, 2.5–5 mL/kg.
Medicines used during neonatal resuscitation
| Medicine and dose | Indications | Effect |
|---|---|---|
|
|
|
|
|
|
|
|
|
Fluid for volume expansion:
|
|
|
If no adequate response has occurred by this stage, a person skilled in neonatal resuscitation should be consulted and the baby transferred with ongoing resuscitation to a higher level of care: -
- Discontinue resuscitation if the unsatisfactory response to resuscitation persists for >20 minutes and underlying conditions e.g. pneumothorax, diaphragmatic hernia has been excluded or >10 minutes of unresponsive cardiac arrest (asystole) and/or >20 minutes of unsustained respiration.
- Babies requiring minimal resuscitation with prompt and complete response may be watched with their mothers.
- Babies with a favourable response to resuscitation should be referred to a neonatal high or intensive care unit, if available, for post resuscitation care.
- Babies, who, after resuscitation, are not completely normal, should be referred to a higher level for care using transport with necessary support, e.g. oxygen, temperature control.