Z29.8
DESCRIPTION
Sexual offences are of grave concern and in particular to the most vulnerable persons including women, children and disabled persons.
The definitions of sexual offences are within the Criminal Law (Sexual Offences and Related Matters) Amendment Act, No 32 of 2007. Sexual offences are physically and psychologically damaging to victims, and the ability to consent to a sexual act depends on the competence of the person to give consent and be knowledgeable of the consequences of that act - including the risk of contracting sexually transmitted diseases such as HIV.
GENERAL MEASURES
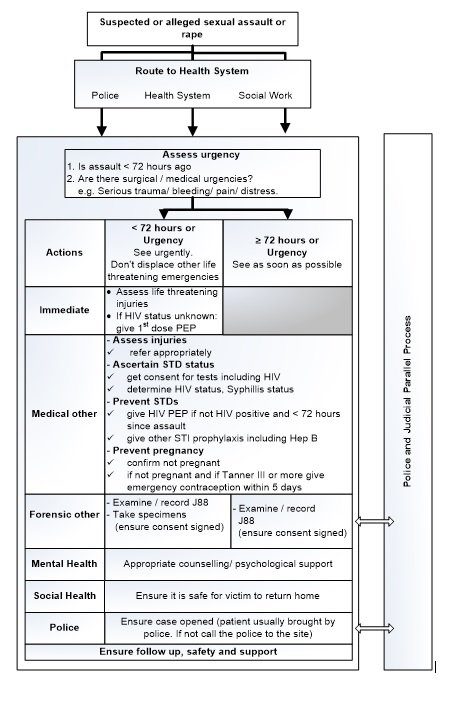
- Sexual offences victims must be regarded as emergencies but do not displace life-threatening management of other cases.
- Ensure appropriate management is in place for every case. So called “cold cases” (> 72 hours after the incident) may be managed medically and given an appointment for medico-legal investigation.
- If the victim wants to open a case, the Family violence, Child protection and Sexual offences Unit (FCS) must be phoned and requested to come to the hospital.
- Cases must be opened in all cases of suspected or alleged rape/sexual abuse in children.
Offer 1st dose of antiretroviral PEP in all cases of suspected rape - the following matters can be resolved in due course:
HIV test
- Determine the patient’s HIV status before initiating PEP.
- Prophylaxis given to a previously infected HIV person will have no clinical benefit and may lead to the development of viral resistance. Provide counselling and manage accordingly.
- Obtain informed consent from the patient and written consent from the parent in case of minors before HIV testing and giving the full course of treatment.
- Consent for HIV testing in children can be given by:
- Children who are competent to give consent and are:
- (i) ≥ 12 years of age; or
- (ii) < 12 years of age and of sufficient maturity to understand the benefits, risks and social implications of such a test.
- Parents or caregivers of children who are not competent to sign consent (but the child should have this explained to them so they understand what is happening, appropriate to their age and development).
- The clinical head of the institution, where a competent person is not available to give consent for HIV testing and PEP (alleged rape in children is a medical emergency).
- Children who are competent to give consent and are:
- Opting for immediate HIV testing remains the patient's choice.
- If the patient declines, give a 3–day starter pack of PEP and encourage the patient to reconsider testing within those 3 days.
- No further PEP should be given in the case of continued refusal of HIV testing in adults, in children where the parent unreasonably refuses PEP this may be taken further.
- If in doubt about the indications for HIV PEP, give PEP.
- A patient presenting after 72 hours since the alleged incident should not be given PEP, but should be counselled about the possible risk of transmission.
- HIV testing should still be offered at the time of presentation and 4 months later.
- If the HIV Elisa/Rapid test is positive in sexually abused children <18 months of age, perform HIV PCR to confirm if HIV infection is truly present.
If HIV-uninfected or if the child has no access to immediate HIV PCR results, they should receive prophylaxis (until the HIV PCR result is obtained).
Pregnancy test
» Perform a pregnancy test in adult and pubertal girls to exclude pregnancy before initiating post exposure contraception and STI prophylaxis.
- Pregnant rape patients should be referred.
Initial Counselling
Counsel all cases of sexual offences patients and caregivers in the case of children
- Explain the side effects of ARVs, e.g. tiredness, nausea and flu-like symptoms.
- Use condoms for 4 months.
- Avoid blood or tissue donation for 6 months.
- Emphasise the importance of compliance with ARV PEP.
- Provide psychosocial support pertaining to:
- Restoring control of the victim by avoiding secondary traumatisation, and give choices and participation in treatment decisions.
- Medical risks, e.g. transmission of sexually transmitted infections including HIV, syphilis, hepatitis-B and C.
- Risk of pregnancy.
- Psycho-emotional-social effects of the sexual assault according to their level of understanding and maturity.
Follow-up support
- Discuss issues relating to stress management at subsequent visits. -
- Inform the patient of the signs and symptoms of post-traumatic stress, syndrome (PTSD), that may eventually cause exhaustion and illness. These include:
- general irritability
- trembling
- pain in neck and/or lower back
- change in appetite
- change in sleep pattern
Medico-legal assessment of injuries
- Complete appropriate required forms and registers.
Investigations
- The patient/parent should sign a consent form for both HIV testing and PEP. Voluntary rapid HIV testing should be made available and should be done on all opting for PEP.
- Further baseline and follow-up investigations are the same as for occupational HIV exposure, with the addition of pregnancy testing in all women and female adolescents prior to post exposure contraceptio. See: secion hypoglycaemia and hypoglycaemic coma and section post-exposure prophylaxis, occupational
MEDICINE TREATMENT.
Prevent the following:
- HIV
- Hepatitis B
- Pregnancy
- STIs
Note:
- Obtain consent for HIV testing from all patients before initiating PEP.
- Offer PEP if the patient presents within 72 hours of being raped and is HIV-uninfected or HIV status is unknown.
- Initiate therapy as early as possible after the exposure to maximize the chance of effective prophylaxis.
- It is important to manage the medical condition before medico-legal examination. Most of these will require referral.
- If, for practical reasons, a person cannot return for the 3-day follow up, a 28-day course of ART should be provided.
HIV PEP
- Therapy may be given up to 72 hours after exposure.
- In children < 18 months of age: initiate antiretroviral PEP while awaiting transfer and HIV PCR results.
Children
- Zidovudine, (AZT) oral, 12 hourly for 28 days.
- Paediatric dose: 180–240 mg/m2. See paediatric dosing tool.
- Maximum: 300 mg/dose.
AND
- Lamivudine, (3TC), oral, 4 mg/kg 12 hourly or 8mg/kg daily for 28 days.
- Maximum: 150 mg/dose if given 12 hourly or 300 mg/dose if given daily. See paediatric dosing tool.
AND
- Lopinavir/ritonavir, (LPV/r), oral 12 hourly for 28 days.
- Paediatric dose: 300/75mg/m2. See paediatric dosing tool.
- Maximum: 400/100 mg/dose.
Dosages may vary by±1 mg/kg/dose, to allow a convenient volume of medication.
Use the adult dosage regimen if children require more than the maximum dose.
Follow-up visits should be at 2 weeks, 6 weeks, and 4 months after the rape.
Adults
Management for HIV prevention is the same as for occupational HIV exposure. See Post-exposure prophylaxis, occupational.
Hepatitis B prevention
Management for Hepatitis B prevention is the same as for occupational hepatitis B exposure. See Post-exposure prophylaxis, occupational.
Emergency contraception (after pregnancy is excluded)
Do a pregnancy test in all women and female adolescents.
Children must be tested and given emergency contraception from Breast Tanner Stage III, if unsure of staging, give emergency contraception when you detect any breast development (DO NOT REGARD MENARCHE AS AN INDICATION). Refer all pregnant rape victims.
- Levonorgestrel oral, 1.5 mg as a single dose as soon as possible after unprotected intercourse.
- Repeat the dose, if the patient vomits within 2 hours.
CAUTION
Emergency contraceptive tablets must be taken as soon as possible, preferably within 72 hours of unprotected intercourse, and not later than 5 days. Women on enzyme inducers (including efavirenz, carbamazepine) cause a significant reduction in levonorgestrel concentrations. Women on these medicines should preferably have copper IUCD inserted or alternatively double the dose of levonorgestrel, because of significant reduction of levonorgestrel. See Contraception, emergency
LoE: III [31]
An anti-emetic:
Adults
- Metoclopramide oral, 10 mg 8 hourly as needed
- STI prophylaxis
Adults
- Ceftriaxone, IM, 250 mg as a single dose.
- For ceftriaxone IM injection: Dissolve ceftriaxone 250 mg in 0.9 mL lidocaine 1% without epinephrine (adrenaline).
AND
- Azithromycin, oral, 1 g, as a single dose.
AND
- Metronidazole, oral, 2 g immediately as a single dose.
Children
Prior to hospital referral, administer:
Children < 45 kg
- Macrolide, e.g.:
- Azithromycin, oral, 20 mg/kg/dose, as a single dose, and refer.
| Use one of the following: | Use one of the following: | Use one of the following: | |||
| Tablet | Tablet | ||||
|
Weight kg |
Dose mg |
Susp 200 mg/5mL |
250 mg | 500 mg |
Age Months/years |
| >7–9 kg | 160 mg | 4 mL | >6-12 months | ||
| ˃9–11 kg | 200 mg | 5 mL | – | – | ˃12–18 months |
| ˃11–14 kg | 240 mg | 6 mL | – | – | ˃18 months–3 years |
| ˃14–18 kg | 320 mg | 8 mL | – | – | ˃3–5 years |
| >18-25 kg | 400 mg | 10 mL | – | – | >5-7 years |
| ˃25–35 kg | 500 mg | – | 2 tablets | 1 tablet | ˃7–11 years |
| ˃35–45 kg | 750mg | – | 3 tablets | – | ˃11–13 years |
| > 45 kg | 1000 mg | – | – | 2 tablets | >13 years |
Children ≥ 45 kg
- Macrolide, e.g.:
- Azithromycin, oral1g, as a single dose, and refer.
AND
- Metronidazole, oral, as a single dose, and refer.
| 1–3 years | 500 mg |
| 3–7 years | 600–800 mg |
| 7–10 years | 1 g |
| > 10 years | 2 g |
AND
- Ceftriaxone, IM, 80 mg/kg/dose immediately as a single dose . See paediatric dosing tool.
- Do not inject more than 1 g at one injection site.
CAUTION :
USE OF CEFTRIAXONE IN NEONATES AND CHILDREN
- If SUSPECTING SERIOUS BACTERIAL INFECTION in neonate, give ceftriaxone, even if jaundiced.
- Avoid giving calcium-containing IV fluids (e.g. Ringer Lactate) together with ceftriaxone:
- If ≤ 28 days old, avoid calcium-containing IV fluids for 48 hours after ceftriaxone administered.
- If > 28 days old, ceftriaxone and calcium-containing IV fluids may be given sequentially provided the giving set is flushed thoroughly with sodium chloride 0.9% before and after.
- Preferably administer IV fluids without calcium contents.
- Always include the dose and route of administration of ceftriaxone in the referral letter
REFERRAL
- All patients with severe physical or psychological injuries.
- All Children: for medico legal and general care assessment after initiation of PEP as outlined above at PHC.
If uncertain, phone Childline 0800055555 - Pregnant rape victims.
- Adults with:
- Active bleeding
- Multiple injuries
- Abdominal pain
- History of the use of a foreign object
- All Children: for medico legal and general care assessment after initiation of PEP as outlined above at PHC.
Note: Refer if there are inadequate resources with regards to:
- counselling
- medico-legal examination
- laboratory for testing
- medicine treatment