T30.0/T31.0-9 + (Y34.99)
DESCRIPTION
Burns lead to skin and soft tissue injury and may be caused by:
- heat, e.g. open flame, hot liquids, hot steam,
- chemical compounds,
- physical agents, e.g. electrical/lightning or
- radiation.
The extent and depth may vary from superficial (epidermis) to full-thickness burns of the skin and underlying tissues. Initially, burns are usually sterile.
Assessment of burns
|
Depth of burn wound |
Surface/colour |
Pain sensation/ healing |
|---|---|---|
|
Superficial or epidermal |
Dry, minor blisters, erythema |
- Painful - Heals within 7 days |
|
Partial thickness superficial or superficial dermal |
Blisters, moist |
- Painful - Heals within 10–14 days |
|
Partial thickness deep or deep dermal |
Moist white or yellow slough, red mottled |
- Less painful - Heals within a month or more Generally needs surgical debridement and skin graft |
|
Full thickness (complete loss of skin) |
Dry, charred whitish, brown or black |
- Painless, firm to touch - Healing by contraction of the margins (generally needs surgical debridement and skin graft) |
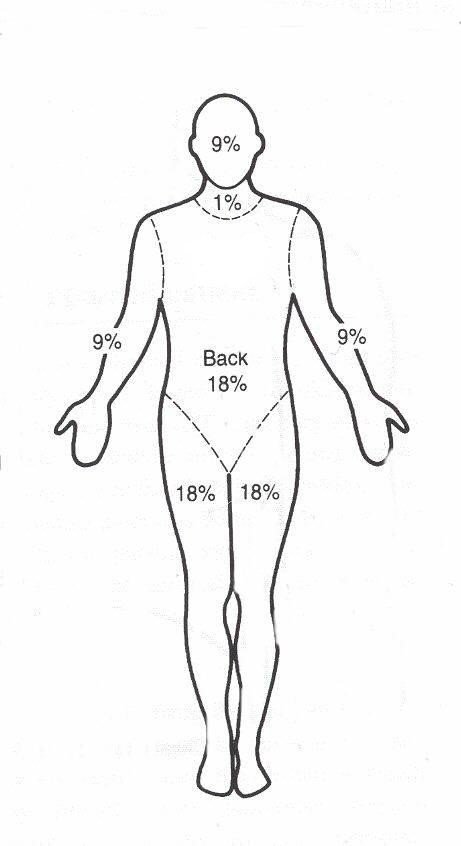
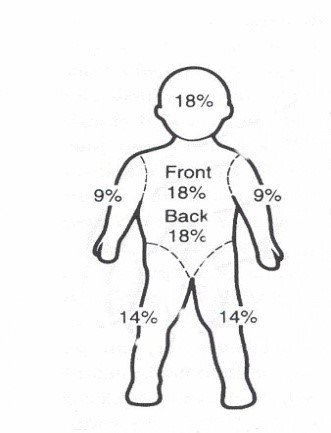
The figures below are used to calculate body surface area %.1
These diagrams indicate percentages for the whole leg/arm/head (and neck in adults) not just the front or back.
In children the palm of the hand, including the fingers, 1%.
Children 8 years and adults
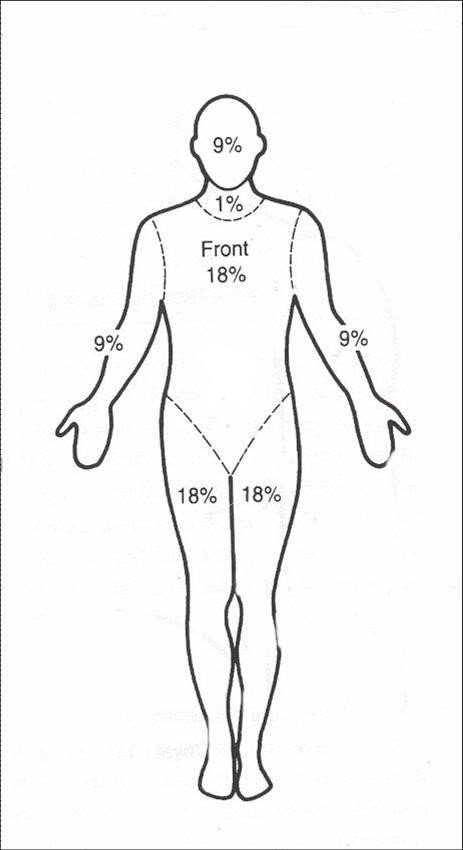
Children 8 years and adults
Children < 8 years of age
1 Source: Karpelowsky JS, Wallis L, Madaree A, Rode H; South African Burn Society..South African Burn Society burn stabilisation protocol. S Afr Med J. 2007 Aug;97(8):574-7.https://www.ncbi.nlm.nih.gov/pubmed/17966146
Child and adult percentages
|
Age years |
Head + neck Front + back |
Torso Front |
Torso Back |
Leg + foot Front + back |
Arm+ hand Front+ back |
|---|---|---|---|---|---|
| < 1 | 18% | 18% | 18% | 14% | 9% |
| 1 - < 2 | 17% | 18% | 18% | 14.5% | 9% |
| 2 - < 3 | 16% | 18% | 18% | 15% | 9% |
| 3 - < 4 | 15% | 18% | 18% | 15.5% | 9% |
| 4 - < 5 | 14% | 18% | 18% | 16% | 9% |
| 5 - < 6 | 13% | 18% | 18% | 16.5% | 9% |
| 6 - < 7 | 12% | 18% | 18% | 17% | 9% |
| 7 - < 8 | 11% | 18% | 18% | 17.5% | 9% |
| ≥ 8 | 10% | 18% | 18% | 18% | 9% |
EMERGENCY TREATMENT
Follow the 7C’s:
- Clothing: remove non-sticking clothing especially if hot or smouldering or constrictive (e.g. rings).
- Cool: with tap water for 30 minutes.
- Clean: with chlorhexidine.
- Cover: with a non-adherent dressing.
- Comfort: provide pain relief.
- Carbon dioxide poisoning: consider if enclosed fire, decreased LOC, disorientation.
- Consider inhalation injury if: carbonaceous (black-coloured) sputum, shortness of breath, perioral burns, hoarse voice stridor. Discuss with referral centre as early intubation may be needed.
MEDICINE TREATMENT
Fluid replacement
- Burns ≤ 10% Total Body Surface Area (TBSA):
- Oral fluids.
- Burns >10% of TBSA:
- IV fluid for resuscitation, replacement and maintenance.
Calculation of fluid replacement
Fluids in adults
If shocked, see Shock .
Replacement fluids for burns
First 24 hours:
- Sodium chloride 0.9%, IV.
- Calculate total fluid requirement in 24 hours:
- Total % burn x weight (kg) x 4 mL.
- Give half this volume in the first 8 hours
- Administer remaining fluid volume in next 16 hours.
- Calculate total fluid requirement in 24 hours:
Note: If urine output is not adequate, increase fluids for the next hour by 50%. Continue at a higher rate until urine output is adequate, then resume normal calculated rate.
Fluids in children
Replacement fluids for burns
- First 8 hours:
Note: Avoid circumferential taping when securing infusion lines, as oedema under the eschar may decrease the venous return.
|
Fluid volume (mL per hour) for the 1st 8 hours in burns of > 10% seen in PHC clinics while awaiting transfer: |
| Burns percentage of total body area |
|
Weight kg |
10–20% | >20–30% | >30–40% | >40% |
| >2–2.5 kg | 15 | 19 | 23 | 28 |
| >2.5–3.5 kg | 20 | 25 | 31 | 36 |
| >3.5–5 kg | 28 | 36 | 44 | 51 |
| >5–7 kg | 40 | 50 | 62 | 73 |
| >7–9 kg | 53 | 70 | 84 | 100 |
| >9–11 kg | 67 | 85 | 105 | 120 |
| >11–14 kg | 82 | 105 | 125 | 150 |
| >14–17.5 kg | 95 | 125 | 155 | 185 |
| >17.5–25 kg | 115 | 155 | 190 | 235 |
| >25–35 kg | 147 | 200 | 250 | 310 |
- Next 16 hours:
|
Fluid volume (mL per hour) for the 2nd (next) 16 hours in burns of > 10% seen in PHC clinics if transfer has not been accomplished in the 1st 8 hours: |
| Burns percentage of total body area |
|
Weight kg |
10–20% | >20–30% | >30–40% | >40% |
| >2–2.5 kg | 12 | 14 | 17 | 19 |
| >2.5–3.5 kg | 16 | 19 | 22 | 25 |
| >3.5–5 kg | 23 | 27 | 31 | 35 |
| >5–7 kg | 33 | 38 | 44 | 49 |
| >7–9 kg | 43 | 50 | 58 | 65 |
| >9–11 kg | 54 | 64 | 72 | 82 |
| >11–14 kg | 64 | 76 | 86 | 97 |
| >14–17.5 kg | 75 | 91 | 104 | 118 |
| >17.5–25 kg | 91 | 110 | 129 | 148 |
| >25–35 kg | 110 | 138 | 165 | 190 |
Pain:
Children
- Paracetamol, oral, 10–15 mg/kg/dose 6 hourly when required. See paediatric dosing tool.
Adults
- Paracetamol, oral, 1 g 4–6 hourly when required.
- Maximum dose: 15 mg/kg/dose.
- Maximum dose: 4 g in 24 hours.
Severe pain:
Wound cleansing:
- Clean the burn wound gently.
- Sodium chloride 0.9% or clean water.
Burn dressing:
For patients requiring referral:
Keep the wound clean and dress with sterile dressings.
For patients requiring referral
- If within 12 hours, transfer patient wrapped in clean dry sheet and blankets.
- If delayed by > 12 hours, paraffin gauze dressing and dry gauze on top.
- For full thickness and extensive burns cover with a paraffin gauze occlusive dressing. Cover the dressing with plastic wrap (e.g. cling film).
For patients not requiring transfer (burns that can be treated at home) :
- Paraffin gauze dressing.
If infected burn :
- Povidone-iodine 5%, cream, applied daily.
Tetanus prophylaxis: Z23.5
If not vaccinated within the last 5 years
- Tetanus toxoid (TT), IM, 0.5 mL.
See Animal bites or Human bites , for detailed indications and management principles.
REFERRAL
- All children < 1 year of age.
- All burns > 5% in children1–2 years of age.
- Full thickness burns of any size in any age group.
- Partial thickness burns > 10% TBSA.
- Burns of special areas – face, hands, feet, genitalia, perineum and major joints.
- Electrical burns, including lightning injury.
- Chemical burns.
- Inhalation injury – fire or scald injury.
- Circumferential burns of the limbs or chest.
- Burn injury in a patient with pre-existing medical disorders which could complicate management, prolong recovery or affect mortality.
- Any patient with burns and concomitant trauma.
- Suspected child abuse.
- Burns exceeding the capabilities of the referring centre.
- Septic burn wounds.
Note: IV fluid replacement is very important in large burns. However, if unable to obtain IV access, give fluids orally or via NGT and transfer urgently.