G40.0-9
DESCRIPTION
Epilepsy is defined as recurrent seizures. Epilepsy is associated with many psychological, social and legal problems, and cultural misperceptions.
DIAGNOSIS
- Is usually made clinically.
- Requires an accurate witness description of the seizure.
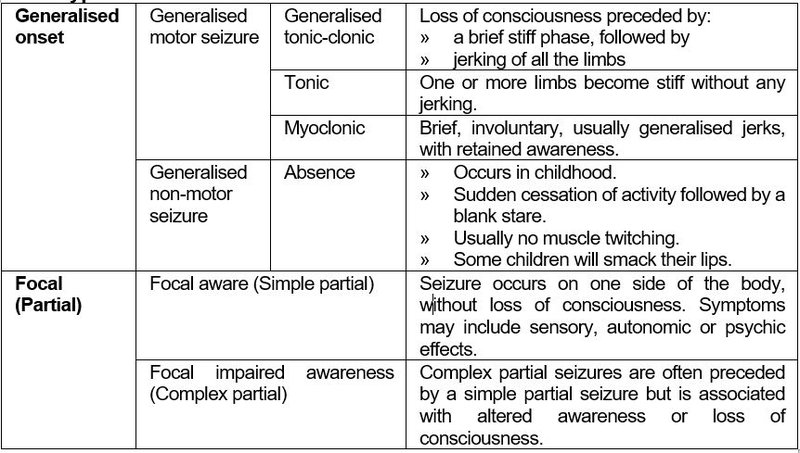
Some types of seizures
GENERAL MEASURES
- Educate patient.
- Advise patient to:
- Record the dates and, if possible, the times of the seizures, in a seizure diary.
- Present the seizure diary at each consultation for assessment of therapy.
- Carry a disease identification bracelet, necklace or card.
- Monitor patients for psychiatric disturbances, intellectual disability (limitations in reasoning, learning and problem solving), anxiety and/or depression, and manage.
- Counsel and advise patient on:
- the adverse effect of alcohol on seizures
- the effect of missing a dose of medication
- the risks of discontinuing medicine treatment without advice of the doctor
- the need for family planning
Counsel the patient about driving, working at heights, swimming and operating machinery. The patient should sign in the notes that they have received this advice.
MEDICINE TREATMENT
Note:
- General rule: a single medicine is best.
- Combination therapy should be initiated only by a specialist.
- Recommended doses are general guides and will be effective in most patients.
- Some patients may need much higher or lower doses. Doses should be increased at 2-weekly intervals only.
- In patients receiving any anticonvulsants, therapeutic drug monitoring may be useful to confirm suspected non-adherence, or diagnose toxicity in a symptomatic patient.
- Therapeutic drug monitoring should be done in patients receiving higher than usual doses of phenytoin.
Medicine interactions
Phenytoin, phenobarbitone and carbamazepine are potent enzyme inducing agents and should be used with caution with other medicines metabolised by the liver, especially warfarin, antiretrovirals, progestin subdermal implants and oral contraceptives.
- Progestin-only injectable contraceptives or IUCDs are the preferred contraceptive methods for women of child-bearing potential on anti-epileptic medication. See Family planning.
LoEIII [4]
Generalised tonic-clonic seizures
Adults
The aim is to use monotherapy, i.e. a single anticonvulsant, progressively increasing the dose until the seizures are controlled or clinically important side effects occur.
- Lamotrigine, oral (Doctor initiated).
- Usual maintenance dose: 100–200 mg daily as a single dose or divided doses.
- Dose-titrate as per table below:
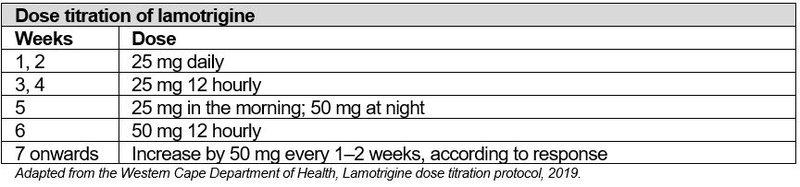
If therapy is interrupted for more than a week, restart the titration protocol. LoEIII:[6]
Note: Carbamazepine and lamotrigine are the preferred anticonvulsants in women of child-bearing potential. Avoid valproic acid in women of child-bearing potential.
CAUTION
Children born to women taking valproic acid are at significant risk of birth defects (10%) and persistent developmental disorders (40%).
Valproic acid is contra-indicated and should be avoided in pregnancy and women of child-bearing potential.
OR
- Carbamazepine, oral (Doctor initiated).
- 100 mg 12 hourly for one week then, 200 mg 12 hourly.
- Titrate upwards by 100–200 mg daily, every week according to response to a maximum dose of 600 mg 12 hourly.
If the initial medicine fails to achieve satisfactory control with optimal dosages, or causes unacceptable adverse effects, then a 2nd medicine may be started. The 1st medicine should be continued for 2 weeks and then gradually reduced over 6–8 weeks until stopped.
Only if already well controlled on phenytoin, continue with:
- Phenytoin, oral, 4.5–5 mg/kg daily on lean body mass, at night (Doctor initiated).
- Phenytoin is a useful and effective agent. However, doses > 300 mg/day are potentially toxic, and could lead to permanent cerebellar damage. Increased dosages should be monitored carefully, both clinically and by medicine concentrations.
Children
The decision to initiate long-term therapy is generally made if the child has experienced ≥ 2 unprovoked convulsions (except febrile convulsions).
- Phenobarbital and carbamazepine are both effective in generalised tonic-clonic seizures.
- Monitor the behaviour profile and academic performance of children on phenobarbital. Change treatment if any problems are identified.
- Phenobarbital, oral, 3.5–5 mg/kg at night (< 6 months of age) (Doctor prescribed).
OR
- Carbamazepine, oral (Doctor prescribed)
Children ≤ 12 years of age:
- Initial dose:
- Syrup (100 mg/5mL): 5 mg/kg/day, given in divided doses, 8 hourly.
- Tablets (200 mg): 5 mg/kg/day, given in divided doses, 12 hourly.
- Depending on response to treatment, increase slowly by 5 mg/kg/day, if necessary, at 2 weekly intervals to a maximum of 20 mg/kg/day or 1 g/day.
- Maintenance dose:
- Maintenance total daily dose: 10–20 mg/kg/day.
Note:
- All children not controlled on carbamazepine 20 mg/kg/day should be referred.
- Carbamazepine may exacerbate myoclonic seizures and absence seizures.
HIV-infected individuals on ART
Children
For HIV-infected children on ART, valproic acid is preferred because of fewer medicine interactions. When switching to valproic acid, commence valproic acid with maintenance dose of the medicine as below and discontinue the other anticonvulsant gradually 7 days. Exclude liver dysfunction prior to initiating therapy (at least ALT), in children < 2 years or if clinical suspicion of liver dysfunction.
- Valproic acid, oral, 5 mg/kg 12 hourly (Doctor prescribed).
- Titrate according to response over 4 weeks up to 15 mg/kg 12 hourly.
- If poorly tolerated divide total daily dose into 3 equal doses.
- Maximum daily dose 40 mg/kg/day.
- Switch to an alternate anticonvulsant when girls reach child-bearing age.
Adults
For HIV-infected adults on ART, lamotrigine is preferred because of fewer medicine interactions. When switching to lamotrigine, commence treatment as below and discontinue the other anticonvulsant after 28 days.
- Lamotrigine, oral (Doctor initiated)
- 25 mg daily for 2 weeks.
- Then 50 mg daily for 2 weeks.
- Thereafter, increase by 50 mg every 2 weeks according to response.
- Usual maintenance dose: 100–200 mg/day as a single dose.
Note: Lamotrigine does not have interactions with dolutegravir. However, the dose of lamotrigine will need to be doubled when patients are switched from efavirenz- or nevirapine-based ART to lopinavir/ritonavir-based ART because the metabolism of lamotrigine is induced by lopinavir/ritonavir.
Poorly controlled epilepsy
Ask the patient, and if possible a family member or primary care giver, about the following, as these factors can influence decisions regarding medicine therapy:
- Has the patient been adherent in taking the medication regularly for at least 2 weeks or more before the seizure? Ask about medicine dosage and frequency.
- If non-adherence has been established, ask for reasons contributing to non-adherence and offer guidance.
- Has the patient recently used some other medicine (i.e. look for drug interactions, substance abuse or traditional medicine use).
- Is there a chance that alcohol is involved?
If ≥ 1 of the above are present, address the problem/s but leave anticonvulsant therapy unchanged (unless dose adjustment is necessary because of a drug interaction). Reassess the patient within 2 weeks.
REFERRAL
- All patients with new onset epilepsy for further investigations such as CT scans.
- Patients with seizures other than generalised tonic-clonic seizures, including absence seizures.
- Increased number of seizures despite attempts to address adherence issues, or changes in the seizure type.
- Patients who have been seizure free on therapy for ≥2 years to review therapy and consideration for stopping treatment.
- Pregnancy.
- Women of child-bearing potential who are on valproic acid for a switch to a less teratogenic medicine.
- Development of neurological signs and symptoms.
- Adverse medicine reactions or suspected toxicity in children.
- If uncontrolled on monotherapy, once patient has been shown to be adherent on monotherapy at the optimal dose.
Information on the seizures that should accompany each referral case.
- Number and frequency of seizures per month (or year).
- Date and time of most recent seizures.
- Detailed description of the seizures, including:
- aura or warning sign
- what happens during the seizure? (give a step-by-step account)
- is the person conscious during the seizure?
- how long do the seizures last on average?
- what does the patient experience after the seizure?
- how long does this experience last?
- Is there a family history of seizures?
- What is the initial date of diagnosis?
- Is there evidence of alcohol use?
- Is there another medical condition, e.g. diabetes, HIV and what medication is used?
- What is the name and dosage of the anti-epileptic medicines used to date?
- Does the person return regularly for repeat of medication?