I10
DESCRIPTION
A condition characterised by an elevated BP measured on three separate occasions, a minimum of two days apart.
However, when BP is severely elevated (refer to table below), a minimum of 3 BP readings must be taken at the 1st visit to confirm hypertension. Ensure that the correct cuff size is used in obese patients.
- Systolic BP ≥ 140 mmHg
and/or
- Diastolic BP ≥ 90 mmHg.
LEVELS OF HYPERTENSION IN ADULTS
| Level of hypertension | Systolic mmHg | Diastolic mmHg |
|---|---|---|
| mild | 140-159 | 90-99 |
| moderate | 160-179 | 100-109 |
| severe | ≥180 | ≥110 |
Achieve and maintain target BP: Systolic < 140 mmHg and diastolic < 90 mmHg.
MONITORING
At every visit:
- Weight
- Blood pressure
Baseline:
- Urine protein by dipstix.
- If dipstix positive send blood for serum creatinine concentration (and eGFR). See Acute kidney injury.
- BMI for cardiovascular risk assessment. See Prevention of ischaemic heart disease and atherosclerosis.
- Abdominal circumference.
- Serum potassium concentration, if on ACE-inhibitor or eGFR < 30 mL/min. See Type 2 Diabetes Mellitus, Adults.
Six monthly:
- Serum potassium concentration in patients on spironolactone or eGFR<30 ml/min.
Annually:
- Fingerprick blood glucose (See: Type 2 Diabetes Mellitus, Adults).
- Urine protein by dipstix (See: Chronic Kidney Disease (CKD)).
- Serum creatinine concentration (and eGFR) in patients who have:
- proteinuria 1+ or more
- existing cardiovascular disease
- hypertension present for 10 years or more (annually if uncontrolled)
- chronic kidney disease (eGFR < 60 ml/min)
GENERAL MEASURES
Screen all patients for cardiovascular disease risk factors (See: Prevention of ischaemic heart disease and atherosclerosis) and prescribe a statin if required.
Screen for presence of compelling indications (see table below) and manage patients accordingly.
Lifestyle modification:
All persons with hypertension should be encouraged to make the following lifestyle changes as appropriate.
- Smoking cessation.
- Maintain ideal weight, i.e. BMI < 25 kg/m². Weight reduction in the overweight patient.
- Salt restriction with increased potassium intake from fresh fruits and vegetables (e.g. remove the salt from the table, gradually reduce added salt in food preparation and avoid processed foods). Dietician’s advice recommended.
- Reduce alcohol intake to no more than 2 standard drinks per day for males and 1 for females.
- Follow a healthy eating plan i.e. low fat, high fibre and unrefined carbohydrates, with adequate fresh fruit and vegetables. Dietician’s advice recommended.
- Regular moderate aerobic exercise, e.g. 40 minutes brisk walking at least 3 times a week.
MEDICINE TREATMENT
Initial medicine choices in patients qualifying for treatment are dependent on presence of compelling indications for specific medicines.
Medicine treatment choices without compelling indications
(see table below: Stepwise treatment without compelling indications, for a list of compelling indications and recommendations for treatment for specific medicines).
Advise patient to take medication regularly, including on the day of the clinic visit, but a single missed dose does not account for severe elevations in BP.
Note:
- Check adherence to antihypertensive therapy by doing pill counts and questioning family members.
- The use of fixed dose combination medication for control of hypertension provides greater adherence and such agents should be used when they are available. LoE:III [39]
- There is emerging evidence that taking the total daily dose of antihypertensive medication at bedtime rather than on awaking provides both better control of hypertension and a significant reduction in important cardiovascular events. LoE:III [40]
- Monitor patients monthly and adjust therapy if necessary until the BP is stable.
- Check adherence to medication before escalating therapy.
- After target BP is achieved, patients may be seen at 3–6 monthly intervals.
Mild hypertension
When there are no cardiovascular risk factors, initiate lifestyle modification measures (Step 1). . If there is poor response to lifestyle modification measures after 3 months, initiate medicine therapy. (Step 2).
If mild hypertension with the presence of risk factors (See: Prevention of ischaemic heart disease and atherosclerosis ),
initiate medicine therapy as well as lifestyle modification (Step 2).
Moderate hypertension
Confirm diagnosis within 2 weeks. Initiate treatment after confirmation of diagnosis (medicine and lifestyle modification) at Step 2.
Severe hypertension
Confirm diagnosis within 1 hour.
- In patients who are not symptomatic, initiate treatment (medicine and lifestyle modification) at Step 3.
Patients with symptoms of progressive target organ damage or associated clinical conditions: See hypertensive urgency and emergency, below and Hypertensive emergency.
Special cases
Pregnancy-induced hypertension
See: Hypertensive disorders of pregnancy
Asymptomatic severe hypertension
- These patients have severe hypertension, are asymptomatic and have no evidence of progressive target organ damage.
- Observe the patient in the health care setting and repeat BP measurement after the patient has rested for 1 hour.
- If the second measurement is still elevated at the same level, start oral treatment with 2 agents (Step 3), one of which should be low dose hydrochlorothiazide and the second medicine is usually a calcium channel blocker, e.g. amlodipine.
- Patient should be followed up within a week.
- Refer to doctor if BP >160/100 mmHg after 4 weeks.
Hypertensive urgency
- Most adults have a systolic BP > 180 mmHg and/or diastolic BP > 110 mmHg.
- Patients are symptomatic, usually with severe headache, shortness of breath and oedema, but there are no immediate life threatening neurological or cardiac complications such as are seen in the hypertensive emergencies (See: Hypertensive emergency).
- Treatment should be commenced with 2 oral agents (Step 3) with the aim to lower diastolic BP to 100 mmHg slowly, over 48–72 hours.
- Amlodipine and furosemide or hydrochlorothiazide should be used, if there is renal insufficiency or evidence of pulmonary congestion (See: Cardiac failure, congestive (CCF), adults).
- All patients with hypertensive urgency should be referred to a hospital.
Stroke
BP is often elevated in acute stroke. Do not treat elevated BP at PHC, but refer patient urgently.
Elderly
In patients without co-existing disease, initiate medicine treatment only when the BP > 160/90 mmHg.
CAUTION
Lower BP over a few days.
A sudden decrease in BP can be dangerous, especially in the elderly.
STEPWISE TREATMENT WITHOUT COMPELLING INDICATIONS
STEP 1: Lifestyle modification.
| Entry to Step 1 | Treatment | Target |
|
AND |
|
|
STEP 2: Add hydrochlorothiazide.
| Entry to Step 2 | Treatment | Target |
|
AND AND OR OR |
AND · LoEI [41] |
|
STEP 3: Add a second antihypertensive medicine.
| Entry to Step 3 | Treatment | Target |
|
OR |
AND ADD OR LoEIII [42] |
|
STEP 4: Increase the dose of the second antihypertensive medicine.
| Entry to Step 4 | Treatment | Target |
|
|
AND AND Increase dose of antihypertensive started in Step 3: OR |
|
STEP 5: Add a third antihypertensive medicine
| Entry to Step 5 | Treatment | Target |
|
|
AND AND AND |
|
STEP 6: Increase the dose of the third antihypertensive medicine
| Entry to Step 6 | Treatment | Target |
|
|
AND AND AND |
with no adverse medicine reactions. |
STEP 7: Increase the dose of HCTZ and add a fourth antihypertensive medicine
| Entry to Step 7 | Treatment | Target |
|
|
AND AND AND AND ADD |
|
CAUTION
Spironolactone can cause severe hyperkalemia and should only be used when serum potassium and renal function can be monitored.Check potassium levels within one month of starting therapy and thereafter, as per clinical need . Routine monitoring of potassium levels is essential if spironolactone is used with an ACE-inhibitor, other potassium sparing agent or in the elderly.
Do not use together with potassium supplements.
Do not use in kidney failure (Do not use if eGFR < 30 mL/min).
If not controlled on step 7– refer.
Hypertension treatment algorithm for stepwise treatment without compelling indications
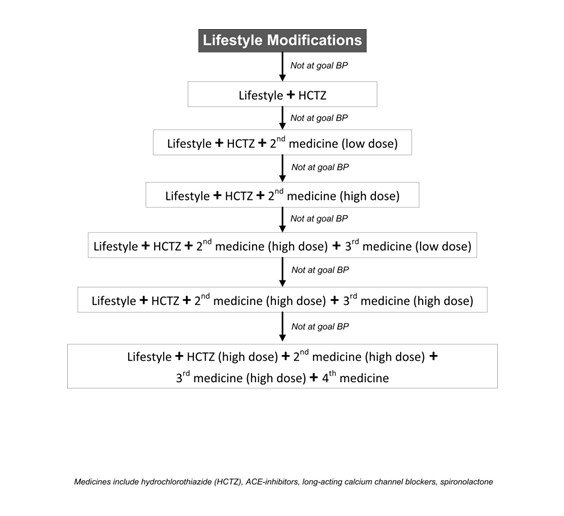
Note:
- If lifestyle modification failed to achieve BP control: Counsel patient on the risk of major cardiovascular events associated with elevated BP; and initiate monotherapy.
- If BP control is suboptimal: Up titrate treatment (maximise dose of current antihypertensive and/or add additional medicine). Evidence suggests that treatment inertia contributes to suboptimal BP control with patients remaining on monotherapy and/or suboptimal doses. LOEIII [45]
- Initiate combination medicine therapy in cases of severe hypertension and hypertension urgency (See: Hypertensive emergency).
| Compelling indications for specific medicines | Medicine therapeutic class |
| Angina |
OR Long-acting calcium channel blocker |
| Prior myocardial infarction |
AND |
| Heart failure |
AND OR Spironolactone, oral For significant volume overload: |
| Left ventricular hypertrophy(confirmed by ECG) |
|
| Stroke: secondary prevention |
AND |
| Diabetes type 1 and 2 with/without evidence of microalbuminuria/proteinuria |
|
| Chronic kidney disease |
|
| Isolated systolic hypertension |
OR |
| Pregnancy |
|
Contraindications to individual medicines
Hydrochlorothiazide
- gout
- pregnancy
- severe liver failure
- kidney failure
- use with caution in patients with a history or family history of skin cancer; and counsel all patients on sun avoidance and sun protection
Spironolactone
- kidney impairment (eGFR<30 mL/min)
- pregnancy
ACE-inhibitors
- pregnancy
- bilateral renal artery stenosis or stenosis of an artery to a dominant/single kidney
- aortic valve stenosis
- history of angioedema
- hyperkalemia
- severe renal impairment (eGFR < 30 mL/min), unless dose-adjusted usage is recommended by a specialist – See: Chronic kidney disease (CKD).
CAUTION
Advise all patients receiving ACE-inhibitors about the symptoms of ACE-induced angioedema.
Calcium channel blockers
- untreated heart failure
REFERRAL
- Young adults (< 30 years of age).
- BP not controlled by 4 medicines and where there is no doctor available.
- Pregnancy.
- Signs of target organ damage e.g. oedema, dyspnoea, proteinuria, angina etc.
- If severe adverse drug reactions develop.
- Hypertensive urgency and hypertensive emergency.