|
Be prepared!
|
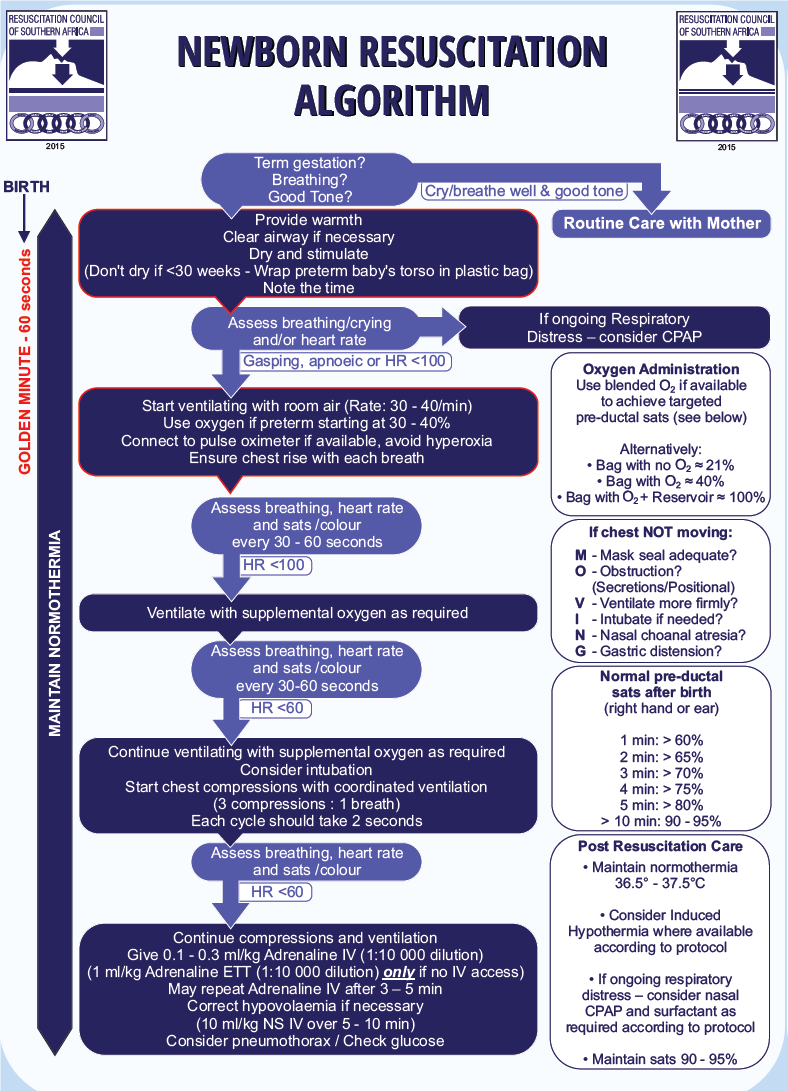
Ask 3 questions to evaluate the infant:
- Is the newborn breathing adequately and not just gasping?
- Is the newborn’s heart rate (HR) above 100 beats per minute?
- Is the newborn centrally pink, i.e. no central cyanosis?
If the answer to all three questions is “yes”, the newborn does not need resuscitation.
If the answer to any of the three questions is “no” the newborn needs resuscitation.
Assess the infant using the above 3 questions every 30 seconds during resuscitation. If the newborn is improving, then the intervention e.g. bagging can be stopped. Only if the baby is not responding or getting worse, is further intervention needed e.g. chest compressions (see algorithm).
Check that each step has been effectively applied before proceeding to the next step. The algorithm follows the assumption that the previous step was unsuccessful and the newborn is deteriorating.
Use the lowest inspiratory oxygen concentration to alleviate central cyanosis and restore a heart rate above 100 beats per minute. There is some evidence that resuscitation with 100% oxygen may be harmful to the baby.
- Oxygen resucitation of newborns
- ≥ 35 weeks gestation: begin with 21%
- < 35 weeks gestation: begin with 21-30%
If baby is breathing but oxygen saturation is not within target range: free-flow oxygen administration may begin at 30%.
An unsatisfactory response to resuscitation includes:
- A sustained slow heart rate, usually less than, or equal to, 60/minute or a progressive decrease in heart rate until cardiac arrest occurs.
- Episodes of cardiac arrest, with a progressively weaker response to chest compressions, positive pressure ventilation and medicines.
- A decreasing blood pressure, increasing acidosis, severe hypotonia with central cyanosis or intense pallor.
- Apnoea or weak, irregular and inefficient respiratory efforts.
- Consider discontinuation of resuscitation if the unsatisfactory response to resuscitation persists for > 20 minutes and underlying conditions e.g. pneumothorax, diaphragmatic hernia has been excluded or > 10 minutes of unresponsive cardiac arrest (asystole) and/or > 20 minutes of unsustainable respiration.
- Admit newborns with a favourable response to resuscitation to a neonatal high or intensive care unit, if available, for post resuscitation care – See section Hypoxia/Ischaemia of the Newborn.
Medicines used during Neonatal Resuscitation
| Medicine | Indications | Dosage | Effect |
|---|---|---|---|
| Adrenaline (epinephrine) |
|
0.1 mL/kg of a 1:10 000 dilution, which may be repeated up to three times ET, 1mL/kg of 1: 10 000 solution |
↑Heart rate ↑Myocardial contractility ↑Arterial pressure |
| sodium bicarbonate (4.2%) (1ml 4,2% = 0.5 mmol Soda Bic) |
|
slow IV, 2–4 mL/kg |
Corrects metabolic acidosis. Improves cardiac output and peripheral perfusion. |
| naloxone |
|
ET/IV/SC/IM, 0.1 mg/kg |
Corrects apnoea and/or hypoventilation. |
|
Fluids: sodium chloride 0.9% |
|
slow IV, (5–10 min)10–20 mL/kg | ↑Blood pressure and improves tissue perfusion. |
| dextrose |
|
IV, 250mg–500 mg/kg (2.5–5 mL/kg of 10% dextrose water) | Corrects hypoglycaemia. |
Published with kind permission from the Resuscitation Council of Southern Africa.