P22.9
DESCRIPTION
Newborn experiencing difficulty with breathing.
Causes of respiratory distress include:
| Pulmonary causes | Extrapulmonary causes |
|---|---|
|
- hyaline membrane disease (surfactant deficiency), - meconium aspiration, - pneumonia, - pneumothorax, - wet lung syndrome, - pulmonary haemorrhage, - pulmonary hypertension, - hypoplastic lungs, and - diaphragmatic hernia. |
- sepsis, - cardiac failure irrespective of cause, - hypothermia/hyperthermia, - hypoglycaemia, - anaemia, - polycythaemia, - hypovolaemic shock, and - perinatal hypoxia. |
Hyaline membrane disease (HMD), meconium aspiration syndrome (MAS) congenital pneumonia and transient tachypnoea of the newborn (TTN) are the most common causes of respiratory distress in newborns.
DIAGNOSTIC CRITERIA
Clinical
- Pulmonary and/or extra pulmonary disorders presenting with two or more of the following signs in a newborn baby:
- tachypnoea (≥60 breaths/minute),
- expiratory grunting,
- intercostal and sternal retractions (recession), and
- central cyanosis while breathing room air.
Investigations
- Chest X-ray to determine underlying pathology.
- Echocardiography, if available, to exclude cardiac causes of respiratory distress.
- Haematocrit, blood glucose and temperature.
- Shake test to assess risk for hyaline membrane disease:
- Within 15 minutes after birth place 0.5 mL gastric aspirate in a clean dry test tube.
- Add 0.5 mL of sodium chloride 0.9% and replace the cap.
- Shake well for 15 seconds.
- Add 1 mL 95% alcohol to the 1 mL mixture of gastric aspirate and sodium chloride 0.9%.
- Replace cap and shake well for 15 seconds.
- Read at 15 minutes.
Interpretation of test:
| Observation | Result | Risk |
|---|---|---|
| No bubbles on surface | Negative | High |
| Incomplete ring of bubbles on surface | Intermediate | Possible |
| Complete ring of bubbles or bubbles covering the entire surface | Positive | Very low |
- In positive test (very low risk of hyaline membrane dsease): surfactant use may not be indicated.
GENERAL AND SUPPORTIVE MEASURES
- Identify and treat underlying cause, e.g.:
- Chest tube and underwater drainage of pneumothorax.
- Isovolaemic dilutional exchange transfusion for symptomatic polycythaemia.
- Admit to neonatal high care/intensive care facility, if available.
- Handle neonate as little as possible.
- Nurse non-intubated infant in the prone position.
- Keep in a neutral thermal environment (incubator or infant crib with overhead heater). Keep room temperature, at 26–28°C, and anterior abdominal wall skin temperature at 36.2–36.8°C.
- Monitor:
- blood pressure,
- respiratory rate,
- peripheral perfusion,
- heart/pulse rate,
- haematocrit,
- acid-base status,
- blood glucose,
- body temperature,
- blood gases,
- SaO₂,
- minerals and electrolytes,
- fluid balance.
- Nutrition:
- Provide adequate IV dextrose to maintain blood glucose ≥ 2.6 mmol/L.
- Commence nasogastric feeding after 12–24 hours if bowel sounds are audible and meconium has been passed.
- If enteral feeding is not possible 24 hours after birth, start IV hyperalimentation.
- Ventilation (non-invasive or invasive) is needed if:
- An oxygen saturation of at least 90% or PaO₂ of at least 60mmHg cannot be maintained with an inspiratory oxygen concentration of ≥ 80% with or without nasal CPAP;
- The PaCO₂ rises to > 55 mmHg with uncompensated respiratory acidosis (pH ≤ 7.20), irrespective of oxygen saturation or PaO₂ .
(1kPa = 7.5 mmHg; 1 mmHg x 0.133 = 1 kPa)
MEDICINE TREATMENT
To eliminate central cyanosis and to maintain oxygen saturation of haemoglobin at 90–94%:
- Oxygen, warmed and humidified via head box, or nasal cannula.
- If a pulse oximeter or facility for blood gas analysis is available oxygen, humidified via head box, or nasal cannulae to maintain oxygen tension in the blood at 60–80 mmHg.
- If a pulse oximeter or facility for blood gas analysis is not available, regulate the inspired oxygen concentration in such a way that the least amount of oxygen that will prevent central cyanosis is used.
- Keep PaO₂ at 60–80 mmHg and PaCO₂ at 35–45 mmHg (arterial blood gas analysis).
Nasal CPAP is needed if the neonate has a good respiratory drive with a PCO₂ of ≤ 55 mmHg but unable to maintain a SaO₂ of 90–94% on an inspiratory oxygen concentration of ≥ 60% (FᵢO₂ ) and pneumothorax has been excluded.
Administer nasal CPAP at 4–6 cm H₂O and monitor SaO₂, blood gas and acid-base status.
OR
- Oxygen/air mixture, hi-flow, warmed and humidified via nasal prongs. (Under specialist supervision)
- Do not exceed 6 L/minute. The flow/minute (L/min) approximates the pressure generated in cm water.
Stabilise circulation and blood pressure
- Neonatal maintenance solution, IV infusion, 60–80 mL/kg/24 hours (day 1 of life) and adapt to daily maintenance requirements.
AND/OR - Sodium chloride 0.9%, 10–20 mL/kg over 1–2 hours.
- For preterm infants restrict to 10 mL/kg.
AND/OR
- For preterm infants restrict to 10 mL/kg.
- Fresh Frozen Plasma, 10–20 mL/kg over 1–2 hours.
OR - Lyphilised Plasma, 10-20 mL/kg over 1-2 hours.
Inotropic support
- Dopamine, IV, 5–15 mcg/kg/minute, continued until blood pressure has stabilised.
- Response to inotropic support will be unsatisfactory if the circulating blood volume is not corrected.
Anaemia
If anaemia is present, Hct < 40 % and Hb <13 g/dL:
- Packed red cells, IV, 10 mL/kg over 1–2 hours.
Metabolic acidosis
If pH ≤ 7.0 and the metabolic acidosis does not respond to normalisation of PaO₂, PaCO₂, blood pressure, volume expansion (hydration) and correction of anaemia:
- Sodium bicarbonate, 4.2 %, IV, administered slowly.
- 1 mmol = 2 mL
- HCO₃ needed (mmol) = base excess x 0.3 x body mass (kg)
- (½ correct base deficit initially)
|
CAUTION
|
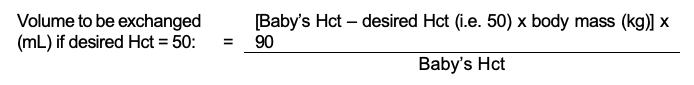
Polycythaemia
Treat with isovolaemic dilutional exchange transfusion using sodium chloride 0.9% if the venous haematocrit is Hct > 65%: Hb >22 g/dL and the baby is symptomatic. Perform under paediatrician’s supervision.
Hyaline membrane disease (Surfactant deficiency)
In consultation with a paediatrician.
Shake test to assess risk for hyaline membrane disease and/or x-ray chest – see above.
If surfactant deficiency is suspected or present, provide respiratory support.
- Mild surfactant deficiency: nasal CPAP 4–6 cm H[2]O.
- Moderate surfactant deficiency: “in-out” surfactant followed by nasal CPAP 4–6 cm H[2]O. Intubate infant and administer surfactant via naso-or orotracheal tube. Ventilate for a few minutes with a T-Piece Resuscitation device or resuscitation bag with a CPAP generating device. Extubate baby and put on nasal CPAP 4–6 cm H[2]O. Babies may be put on nasal CPAP directly after “in-out” surfactant administration, omitting the ventilation step following “in-out” surfactant.
- Severe surfactant deficiency: intubate baby and ventilate with a ventilator. Administer surfactant via the naso- or orotracheal tube. If a ventilator is not available the in-out surfactant followed by nasal CPAP can be used.
Short term intubation (In-out endotracheal surfactant administration)
- Nasal CPAP as required.
- If inadequate oxygenation on nasal CPAP, pre-oxygenate with bag-mask or T-piece ventilation to maintain preductal saturation between 90-94%.
- Intubate orally, give surfactant and follow with gentle manual ventilation or CPAP, as required, for 5 minutes:
- Surfactant, 100mg/kg
- Extubate and recommence nasal CPAP.
Infection
- If infection, e.g. bronchopneumonia, is present or suspected, give antibiotics after blood cultures have been taken.
- Consider the antibiotic sensitivity profile of micro-organisms in a particular hospital when prescribing antibiotics.
- Aminoglycoside, e.g.:
- Gentamicin, IV, for 5-7 days in the first week of life.
- If < 32 weeks gestation of age: 5 mg/kg/36 hours.
- ≥ 32 weeks gestation of age: 5 mg/kg/24 hours.
- After first week, 5 mg/kg/24 hours for all gestations.
PLUS
- Ampicillin, IV, for 5-7days.
- If < 7 days of age: 50 mg/kg 12 hourly.
- If 7 days – 3 weeks of age: 50 mg/kg 8 hourly.
- If > 3 weeks of age: 50 mg/kg 6 hourly.
Review after 72 hours. If infection is confirmed or very strongly suspected continue for 10 days.
Where available, gentamicin doses should be adjusted on the basis of therapeutic drug levels.
- Trough levels (taken immediately prior to next dose), target plasma level < 1 mg/L.
- Peak levels (measured 1 hour after commencement of IV infusion or IM/IV bolus dose), target plasma level > 8 mg/L.
REFERRAL
- No improvement or deterioration despite adequate treatment.
- Development of respiratory failure and need for ventilatory support.