P58
- Description
- Diagnostic criteria
- Breastfeeding associated jaundice
- Hyperbilirubinaemia, unconjugated
- Hyperbilirubinaemia, conjugated
DESCRIPTION
Yellow discolouration of the skin and mucous membranes due to hyperbilirubinaemia.
Bilirubin is formed mainly from haem catabolism. Jaundice develops when there is an overproduction of bilirubin, defective bilirubin metabolism and/or defective excretion of bilirubin from the body.
DIAGNOSTIC CRITERIA
Jaundice may be physiological or pathological.
Physiological jaundice
- Seldom appears before 24–36 hours after birth.
- Rarely lasts more than 10 days in the full term infant and 14 days in the pre-term infant.
- Only the unconjugated bilirubin fraction is increased.
- Total peak serum bilirubin concentration is usually below 275 micromol/L in the term infant.
- Total bilirubin concentration does not rise by more than 85 micromol/L/24 hours or 17 micromol/L/hour.
- The baby thrives and shows no signs of illness or anaemia.
- Treatment is unnecessary.
Pathological jaundice
- May appear within the first 24 hours of birth, but can occur at any time after birth.
- Persists for longer than 10 days in the full term infant or 14 days in the pre-term infant.
- The unconjugated and/or conjugated fractions of bilirubin are increased.
- The conjugated bilirubin level exceeds 20% of the total bilirubin value, or the conjugated bilirubin fraction is 30 micromol/L or more.
- Total bilirubin concentration rises by more than 85 micromol/L/24 hours or 17 micromol/L/hour and the total serum bilirubin level is above physiological level.
- There are signs and symptoms of illness in the baby.
- Stools are pale in obstructive jaundice.
BREASTFEEDING ASSOCIATED JAUNDICE
Increased unconjugated bilirubin levels during the first week of life in breastfed babies is due to calorie and fluid deprivation and delayed passage of stools. Improves with increased frequency of breastfeeding.
HYPERBILIRUBINAEMIA, UNCONJUGATED
| Excessive haemolysis | Defective conjugation |
|---|---|
|
- ABO incompatibility - rhesus disease - enclosed haemorrhages - polycythaemia - infections* - spherocytosis - G6PD deficiency |
- prematurity - infection - hypoxia - hypoglycaemia - hypothyroidism* - breast milk jaundice* |
* may cause prolonged neonatal jaundice.
GENERAL AND SUPPORTIVE MEASURES
- Treat the underlying cause.
- Monitor the infant’s body temperature and maintain within thermoneutral range.
- Maintain adequate nutrition and hydration.
- Correct factors known to increase the risk of brain damage in babies with jaundice e.g.:
- hypoxia,
- prematurity,
- hypoglycaemia,
- hypothermia,
- acidosis,
- hypoalbuminaemia, and
- haemolysis.
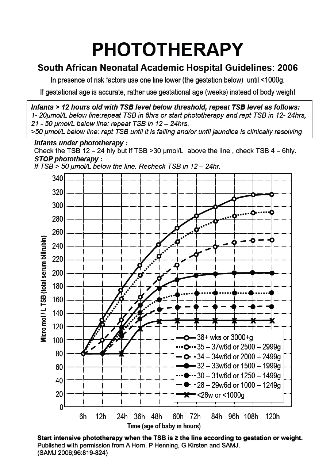
PHOTOTHERAPY
Guideline for initiating phototherapy:
- Commence phototherapy based on total serum bilirubin measurements, correlated with phototherapy graph attached. The need for phototherapy is determined by the level according to hours of life and gestation or weight.
- The skin colour of a baby receiving phototherapy does not reflect the degree of jaundice (bilirubin blood level) or the efficacy of the phototherapy.
- Undress the baby and cover the eyes with gauze pad or commercially available eye covers.
- Position the phototherapy unit (fluorescent light bulbs of 400–500 nm wavelength) not higher than 45 cm above the baby.
- Check spectral irradiance of the fluorescent lights using a radiometer after every 200–300 hours of use to ensure that they are effective.
- The spectral irradiance should be above 10 microwatt/cm²/nm of wavelength. If spectral irradiance cannot be checked regularly, replace fluorescent light bulbs after 1 000 hours of continuous use.
- A quartz halogen light source (400–500 nm wavelength) can also be used for phototherapy.
- Phototherapy units with diodes emitting light in the blue spectrum or fibro-optic phototherapy units can be used instead of the fluorescent/quartz halogen units.
- Terminate phototherapy when the total serum bilirubin level is more than 50 micromol/L below the recommended phototherapy initiating level, and the cause of the jaundice has been determined and adequately addressed.
- A rebound increase in bilirubin may follow termination of phototherapy.
- Monitor bilirubin levels approximately 6 hourly after phototherapy has been stopped.
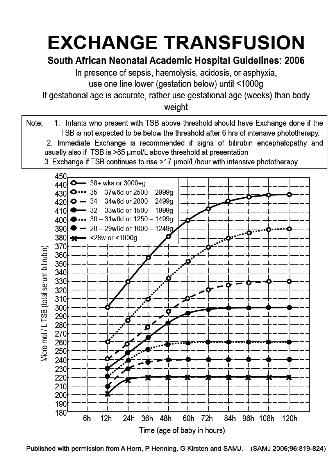
Guideline for exchange transfusion (see also the graphs below):
- Exchange transfusion is indicated when the risk of bilirubin encephalopathy and kernicterus is significant. Referral for exchange transfusion may be needed.
MEDICINE TREATMENT
Rh incompatibility (i.e. mother Rh negative, baby Rh positive).
ABO incompatibility (i.e. mother = O, baby = A, B or AB).
Once the diagnosis of Rh- or ABO-related haemolysis is confirmed, together with a positive direct Coombs test; and the serum bilirubin is rising rapidly ( >17 µmol/hour with intensive phototherapy) or is approaching exchange transfusion level then administer:
- Gammaglobulin, IV, 500 mg/kg over 1 hour (in consultation with a specialist).
- Can be repeated once after 6–8 hours.
Mothers of babies with Rh incompatibility should receive:
- Anti D immunoglobulin, IM, 100 mcg as soon as possible after birth but within 72 hours of birth.
HYPERBILIRUBINAEMIA, CONJUGATED
| Hepatocellular disease | Bile duct obstruction |
|---|---|
|
- hepatitis * - total parenteral nutrition * - syphilis - other congenital infections - galactosaemia* |
- bile duct hypoplasia/atresia* - choledochal cyst - cystic fibrosis |
* May cause prolonged neonatal jaundice.
Conjugated hyperbilirubinaemia is due to intra/extrahepatic obstruction of bile ducts (cholestasis) and usually presents in the second week of life or later.
The baby has a green-yellow skin discolouration, dark bile stained urine and pale acholic stools. Hepatomegaly is commonly present and the infant often fails to thrive.
Neonatal hepatitis, prolonged TPN and biliary atresia or hypoplasia accounts for the majority of cases of conjugated hyperbilirubinaemia.
GENERAL AND SUPPORTIVE MEASURES
- Treat the underlying cause.
- Dietary modifications to counteract the malabsorption of fat and fat soluble vitamins (A, D, E and K) that may occur in patients with a prolonged conjugated hyperbilirubinaemia.
- When galactosaemia is suspected avoid lactose containing feeds, i.e. breast milk and lactose containing formula.
MEDICINE TREATMENT
All premature babies, day 15 to 1 year:
- Multivitamin, oral, 0.6 mL daily.
SURGICAL TREATMENT
Conditions amenable to surgery e.g. biliary artresia.
Hepatoporto-enterostomy for biliary atresia should be done before 60 days of age for optimal outcome.
REFERRAL
- All cases of jaundice persisting more than 2 weeks with conjugated bilirubin level > 20% of total bilirubin, for diagnosis and initiation of treatment.