N18.9
DESCRIPTION
Chronic kidney disease (CKD) is defined as: "evidence of structural or functional kidney abnormalities (abnormal urinalysis, imaging studies or histology) that persist for at least 3 months, with or without a decreased glomerular filtration rate (GFR), as defined by a GFR of less than 60 mL/min/1.73 m²”.
It is characterised by a progressive decline in renal function to end stage renal failure due to progressive loss of functioning glomeruli and is accompanied by the onset or worsening of proteinuria.
A calculated glomerular filtration rate can be ascertained using the height of the child in cm, the serum creatinine (micromol/L) and a factor “K”. (Modified Schwartz formula).
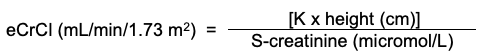
| Value of K | |
|---|---|
| Low birth-weight (<2.5kg) infant | 30 |
| Infant 0 - 18 months | 40 |
| Girls 2 - 16 years | 49 |
| Boys 2 - 13 years | 49 |
| Boys 13 - 16 years | 60 |
Staging of chronic kidney disease (KDQOI definition)
| Stage |
*eGFR (mL/min/1.73 m 2 ) |
Features |
|---|---|---|
| 0 | ≥ 90 | Screening of at risk for CKD patients |
| 1 | ≥ 90 |
Renal parenchymal disease present with normal eGFR - monitor annual |
| 2 | 60-89 |
Usually asymptomatic – biochemical abnormalities present - monitor annually |
| 3 | 30-59 |
Biochemical abnormalities and poor growth, poor appetite - monitor 3-6 monthly |
| 4 | 15-29 |
Severe disease - consider renal replacement therapy |
| 5 | < 15 (ESRF) |
End stage renal failure - consider renal replacement therapy |
*eGFR: estimated glomerular filtration rate
DIAGNOSTIC CRITERIA
Renal function may deteriorate without clinical symptoms.
- Children are likely to present with acute on chronic renal failure during episodes of acute intercurrent illness.
- Poor weight gain and stunting.
- Poor appetite, chronic constipation, polydipsia and polyuria.
- Children with renal tubular disorders or bilateral renal dysplasia have obligatory salt wasting and are often unable to concentrate urine. This may result in severe dehydration and metabolic acidosis if they do not have free access to water.
- May present with tachypnoea mimicking acute “respiratory distress” to compensate for metabolic acidosis.
- Chronic anaemia.
- Renal osteodystrophy, i.e. bone pain and skeletal deformities.
- Volume overload: oedema, hypertension, heart failure, pulmonary oedema.
- Uraemic symptoms and signs: nausea, vomiting, pruritis, brownish skin pigmentation, uraemic frost.
- Bleeding tendency (mucosa).
- Convulsions due to hyponatraemia, hypernatraemia, hypocalcaemia, uraemia or hypertension.
Investigations
- Urine:
- Protein:creatinine ratio is usually increased (normal < 0.02 g/mmol).
- Iso-osmolar, i.e. urine Osmol 300–350 mOsm/L (normal maximal urine concentration > 1000 mOsmol/L).
- Urine volume may be:
- normal, or
- increased (polyuria): > 4 mL/kg/hour, or
- decreased (oliguria): < 1.0 mL/kg/hour.
- Urine test strip:
- May be normal or reveal proteinuria, haematuria, glycosuria.
- Nitrites and leucocytes may indicate UTI. Do urine MCS.
- Urine microscopy
- May be normal or reveal casts.
- Pus cells, leucocyte casts and bacteria may indicate UTI. Do urine MCS.
- Serum urea:
- Increased, depending on hydration, nutritional state and protein intake.
- Serum creatinine is a better indicator of renal function than serum urea but
- It is influenced by age of child and muscle bulk.
- It may be only mildly increased in a malnourished child with little muscle bulk despite advanced renal failure (serum creatinine only starts increasing once renal function has fallen to less than half normal).
- Serum electrolytes:
- Hyperkalaemia.
- Hyperchloraemia and decreased bicarbonate.
- Calcium, phosphate and ALP:
- Decreased calcium.
- Increased phosphate.
- Increased ALP.
- Plasma parathyroid hormone:
- Increased.
- Renal ultrasound:
- To exclude obstruction.
- Small shrunken kidneys are indicative of chronic renal failure.
There is no place for renal biopsy in patients with end stage renal failure.
GENERAL AND SUPPORTIVE MEASURES
- Determine and treat the underlying cause of chronic renal failure.
- Monitor fluid intake and output, and blood pressure.
- Weigh daily.
- If in respiratory distress due to volume overload:
- Place in sitting position.
- Give oxygen, 100%, 2–3 L/minute by nasal prongs.
- Dietary management:
- Monitor potassium closely.
- Limit potassium intake if serum potassium > 5.5 mmol/L.
- Restrict fruit juices, dried fruit, all citrus fruits, bananas, guavas and tomatoes.
- All vegetables should either be soaked for 24 hours before cooking or water should be decanted twice during cooking.
- Restrict phosphate once serum phosphate reaches or exceeds the upper limit of normal for age, usually >1.8 mmol/L and when GFR <70 mL/min/1.73m².
- Limit dairy products and other foods with high phosphate content like grains and cereals, carbonated cool drinks, etc.
- Do not limit protein intake.
- Restrict salt intake. No salt added during preparation of food, no salt on the table during meals and restrict all salt preserved foods.
Generally, salt is restricted for hypertensive, oedematous patients, but not for patients with salt losing nephropathies who are polyuric, unless they are hypertensive. - High-energy diet with supplementary nasogastric feeds or nocturnal fluids for children with poor appetite, polyuria/nocturia and with inadequate intake to maintain growth.
- Fluid management:
- Depends on underlying kidney disease.
- Use body weight to guide fluid prescription.
- Only use parenteral fluids if oral intake is not possible.
- Children with tubular abnormalities may be unable to concentrate their urine and therefore require free access to water.
- Anuric: Fluid to replace insensible water losses only.
Use an electrolyte free solution i.e. dextrose 5% or 10%, IV.
Insensible water loss is calculated as:- Neonate and young baby: 30–40 mL/kg/day.
- Older children: 25 mL/kg/day (400 mL/m²/day).
- Oliguric with oedema and hypertension: Total volume fluid allowed calculated as:
Insensible water loss is calculated as:- Neonate and young baby: 30–40 mL/kg/day.
- Older children: 25 mL/kg/day (400 mL/m²/day).
- Use an electrolyte free solution i.e. dextrose 5% or 10%, IV.
plus
50% of urine output.
plus
Extra-renal losses (volume for volume).
Use a potassium-free solution, e.g. sodium chloride 0.9%.
Once euvolaemic, give same fluids as above to replace 100% of urine output. - Dehydrated and hypotensive: Give sodium chloride 0.9%, IV bolus immediately and re-assess.
Repeat bolus, if necessary.
Strictly monitor urine output and fluid losses.
MEDICINE TREATMENT
Avoid nephrotoxic agents and appropriately adjust renally excreted medicines, e.g. NSAIDs, aminoglycosides, vancomycin, amphotericin B, radiocontrast drugs.
Vitamins and minerals
- Multivitamin, oral, 5 mL daily.
(Formulation to include pyridoxine, other B vitamins, vitamin C 30 mg and vitamin D 400 IU)
AND - Folic acid, oral, 5 mg daily.
For management of hyperphosphataemia/osteodystrophy and hyperparathyroidism:
In combination with restricted dietary intake of phosphate:
- Calcium carbonate, oral, 1–4 tablets chewed 8 hourly with meals.
- 1 tablet is equivalent to 0.168 g elemental calcium.
- Alfacalcidol oral, 0.25 mcg daily. Specialist initiated.
- If serum phosphate is >2.5 mmol/L, treat the hyperphosphataemia first with:
- Dietary modification,
- Calcium (elemental), oral, 10 -15 mg/kg/dose, 12 hourly.
- Maximum dose: 1 000 mg (1g) daily.
- Calcium carbonate 420 mg = 168 mg elemental calcium.
- To decrease to below < 1.8 mmol/L before beginning the alfacalcidol (to avoid metastatic calcification).
In patients with serum calcium < 2.2 mmol/L start alfacalcidiol early:
- Alfacalcidol oral, 0.25 mcg, initially twice weekly. (Specialist initiated)
- Increase dose as necessary to maintain serum calcium in upper normal range.
Chronic metabolic acidosis
If serum bicarbonate < 18 mmol/L:
- Sodium bicarbonate, oral, 1mmol/kg/dose 2–3 doses per day after meals.
- Adjust according to response.
Note: The intravenous formulation can be given orally.
Hyperkalaemia
Discontinue all medicines that may cause hyperkalaemia, e.g. potassium sparing diuretics, spironolactone, ACE inhibitors.
Exclude volume depletion as an underlying cause for hyperkalaemia.
If serum potassium remains > 5.5 mmol/L:
- Sodium polystyrene sulphonate, oral/rectal, 1g/kg/dose in dextrose water, once or twice daily.
- Treat accompanying metabolic acidosis.
Anaemia
Ensure adequate intake of haematinics.
Ensure adequate iron stores. Measure ferritin, transferrin, transferrin saturation and total iron binding capacity.
Avoid transfusions if possible due to risk of developing antibodies in a patient who may be a potential candidate for renal transplantation.
If a patient has symptomatic anaemia, haemoglobin usually < 7g/dL:
- Packed cells, IV, 10 mL/kg administered over 6 hours.
If the patient has a persisting haemoglobin level < 8g/dL despite correction of possible deficiencies of iron, folic acid or vitamin B₁₂ treatment, start recombinant human erythropoietin (rHuEPO) in consultation with a paediatric nephrologist.
Note:
Blood pressure must be controlled before starting rHuEPO treatment.
Dose of erythropoietin is gradually increased according to increase in haemoglobin. Target haemoglobin is 10–12 g/dL.
- Erythropoietin, SC, 75 units/kg/week in divided doses 2–3 times a week.
- Monitor Hb levels every 4 weeks.
- Adjust dose until target haemoglobin level of 12 g/dL is reached. Continue with this dose.
- If the Hb level is increasing, do not change dose.
- If the Hb level remains unchanged, increase by 25% at 4-week intervals until maximum dose of 300 units/kg/week is reached.
- If Hb level increases > 12 g/dL, stop treatment for one week. Thereafter continue with 25% less than previous dose per week.
For persistent anaemia:
Refer to tertiary centre for nephrologist assessment.
Hypertension
See Chapter: Cardiovascular System, Hypertension in children .
Dyslipidaemia
Dyslipidaemia may contribute to the progression of chronic kidney disease, particularly in children with nephrotic syndrome. Hypertriglyceridaemia and abnormal apolipoprotein metabolism is a feature of CRF. Dietary intervention is necessary, including limiting saturated fat and cholesterol intake.
For children > 8 years with persistent total cholesterol levels > 7 mmol/L:
- HMGCoA reductase inhibitors (statins), e.g.:
- Simvastatin, oral, 10 mg at night.
- Maximum dose: 20 mg at night.
Refer for advice on management.
Renoprotective treatment
All children with persistent nephrotic range proteinuria and GFR > 30 mL/minute:
- ACE inhibitor (with nephrologist supervision).
- Enalapril, oral, 0.1mg/kg/dose, once daily.
- Increase dose to 0.5 mg/kg/day, as a single dose or two divided doses.
- Monitor for adverse effects: hyperkalaemia (increased risk when potassium sparing diuretic is used simultaneously) and acute renal failure (increased risk in children with impaired renal function or volume depletion).
- May cause hyperkalaemia, worsening metabolic acidosis and declining renal function while reducing proteinuria.
- Monitor serum urea and electrolytes, i.e. serum potassium and bicarbonate, and renal function within 7 days.
- If serum creatinine has doubled, check hydration status, stop diuretics and halve the dose of ACE inhibitors.
- If renal function does not improve, or hyperkalaemia > 5.5 mmol/L persists, stop ACE inhibitor treatment.
Immunisation
Give all EPI vaccines according to the schedule.
Provide all routine vaccinations or missing vaccinations in older children.
Check immunity against chicken pox and Hepatitis B.
In children > 2 years of age:
- Pneumococcal vaccine (polysaccharide), IM, 0.5 mL as a single dose.
In the absence of any immunity against chickenpox give:
- Varicella-zoster vaccine, SC, 2 doses 6 weeks apart.
In the absence of immunity against Hepatitis B, vaccinate as for any non-immune individual.
- Hepatitis B vaccine, IM, 1mL, 3 doses one month apart.
- If the antibody level is considered non-protective or insufficient, give 2 booster doses one month apart.
REFERRAL
- All children with chronic kidney disease
- Patients with dyslipidaemia or hypercholesterolaemia.