N17.9
- Description
- Diagnostic criteria
- General and supportive measures
- Medicine treatment
- Other complications
- Referral
DESCRIPTION
Acute kidney injury (AKI) is a syndrome characterised by a rapid decline in glomerular filtration rate and retention of fluid and nitrogenous waste products. It often presents as a continuum of volume responsiveness “prerenal AKI” up to a point of volume unresponsiveness. AKI is classified as prerenal, renal and postrenal failure.
Levels of AKI is defined by pRIFLE criteria (mnemonic p=paediatric, Risk, Injury, Failure, Loss and End Stage Renal Failure).
Paediatric modified RIFLE (pRIFLE) criteria
| Level |
Estimated creatinine clearance (eCrCl)* |
Urine output |
|---|---|---|
| 1 | ↓eCrCl by 25 % | <0.5 mL/kg/hour for 8 hours |
| 2 | ↓eCrCl by 50 % | <0.5 mL/kg/hour for >16 hours |
| 3 | ↓eCrCl by 75 % |
<0.5 mL/kg/hour for >24 hours or anuria for 12 hours |
The previous method of measuring creatinine clearance using 24-hour urine sample is not recommended due to the difficulty in obtaining an accurate 24 hour urine collection in children. A calculated glomerular filtration rate can be ascertained using the height of the child in cm, the serum creatinine (micromol/L) and a factor “K”. (Modified Schwartz formula)
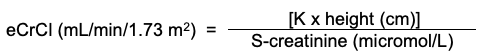
| Value of K | |
|---|---|
| Low birth-weight (<2.5kg) infant | 30 |
| Infant 0 - 18 months | 40 |
| Girls 2 - 16 years | 49 |
| Boys 2 - 13 years | 49 |
| Boys 13 - 16 years | 60 |
Normal values for GFR in children:
| Age | Mean GFR ( ml/min/1.73/ m 2 ) | Range |
|---|---|---|
| Birth | 20 | |
| 7 days | 40 | 25-60 |
| 1 month | 50 | 30-70 |
| 6 months | 75 | 40-100 |
| 12 months | 115 | 65-160 |
| 2-12 years | 125 | 90-165 |
DIAGNOSTIC CRITERIA
Clinical
- In neonates exclude congenital abnormality of the urinary tract.
- Oliguria is the most common manifestation, i.e.:
Neonates: output <1 mL/kg/hour.
Older children: output ≤0.3 mL/kg/hour. - Prerenal: shock and dehydration.
- Postrenal: exclude obstruction, e.g. palpable bladder.
- Intrinsic kidney disease: oedema, volume overload, hypertension.
- Signs of underlying infection/septicaemia, e.g. fever, skin rash, etc.
Investigations
- Urine macroscopic appearance: brownish with acute tubular necrosis.
- Urine test strip: haematuria, proteinuria indicative of glomerular disease; leucocytes and nitrites in favour of pyelonephritis.
- Urine microscopy: red blood cell casts, leukocyte, hyaline and granular casts.
- Urine culture to exclude pyelonephritis.
- Urine biochemistry:
| Pre-renal failure | Intrinsic renal failure | |
|---|---|---|
| U-Osmol (mOsmol/L) | ↑> 320 | equal to serum Osmol |
| FeNa % * | < 1 % | ≥3 % |
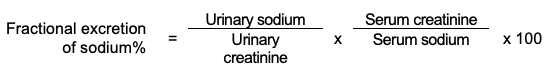
*FeNa % becomes an invalid test for pre-renal failure if the child has received furosemide.
Note: Serum creatinine is measured in micromol/L and urine creatinine in millimol/L. To convert micromol/L to millimol/L ÷ by 1000
- Ultrasound of kidneys and bladder.
- Serum urea, urate, creatinine, electrolytes and osmolarity, glucose, calcium, phosphate and albumin.
- Typical biochemistry: hyperkalaemic metabolic acidosis, hyponatraemia, hypocalcaemia, hyperphosphataemia.
- Full blood count, differential and platelet count.
- Clotting profile.
- Cultures and DIC workup as indicated.
- ECG on to exclude life threatening hyperkalaemia.
- Chest X-ray to evaluate cardiomegaly, pleural effusions and pulmonary oedema.
GENERAL AND SUPPORTIVE MEASURES
- Treat the underlying cause.
- Monitor fluid intake and output, blood pressure.
- Weigh daily.
- Nutritional support.
- High-energy diet. Give supplementary nasogastric feeds, if required. Infants should preferably be given breast feeds or an infant milk formula.
- Daily requirements:
- protein: 1 g/kg maximum
- carbohydrate: 2–3 g/kg
- fat: 2 g/kg
- Restrict NaCl, potassium and phosphate intake.
- Restrict protein intake when S-urea >25 mmol/L.
Avoid nephrotoxic or renally excreted medicines, e.g.
NSAIDs, aminoglycosides, vancomycin, cough and cold mixtures, radiocontrast drugs.
- Fluid management:
- Depends on volume status, urine output and extra-renal losses.
- Never use a potassium-containing solution in an anuric patient.
- Only use parenteral fluids if oral intake is not possible.
IMPORTANT
Fluid balance is critical. Assess at a minimum, every 12 hours to make appropriate changes to fluid prescription.
- Fluid management according to fluid status:
IMPORTANT
Insensible water loss is calculated as:
- Neonates and young babies: 30 - 40 mL/kg/day
Older children: 25 mL/kg/day (400 mL/m²/day)
Pulmonary oedema plus oliguria/anuria: Do not give fluid.
Hydrated anuric patient without extra-renal fluid losses: Oral fluid to replace insensible water losses only.
Normally hydrated plus oliguria: Oral fluid intake to replace insensible water loss plus urine output of previous 24 hours.
Dehydrated, oliguric and ongoing extra-renal fluid losses: Replace fluid losses with an appropriate solution which mirrors losses e.g.:
- for diarrhoea: ½ Darrows/dextrose 5%, IV or oral rehydration solution;
- for vomiting/gastric fluid losses: sodium chloride 0.9%/dextrose 5%.
Normally hydrated plus normal urine output: Give normal fluid intake.
Shock: See Chapter: Emergencies and Trauma, Shock .
Polyuria , (urine output >4 mL/kg/hour): which usually occurs during the recovery (diuretic) phase of acute tubular necrosis: Replace fluid and electrolyte losses with ½ Darrows/dextrose 5%, IV. Volume to replace is equal to urine output of preceding 12 hours.
MEDICINE TREATMENT
Hyperkalaemia
Monitor ECG for signs of hyperkalaemia.
Discontinue all sources of intake of potassium.
Treat when serum potassium >6.5 mmol/L.
Monitor response to treatment and adjust accordingly.
- Calcium gluconate 10 %, IV, 0.5mL/kg/dose slowly over 3–5 minutes.
- Salbutamol, solution, 2.5–5 mg/dose, nebulise over 20 minutes. 0.5–1 mL salbutamol in 2-4 mL sodium chloride 0.9%.
OR Salbutamol, IV, 4 mcg/kg in 5 mL water administered over 30 minutes. - Sodium bicarbonate 4.2%, IV, 4 mL/kg administered over 4 hours.
- Do not mix calcium and sodium bicarbonate-containing solutions.
Check Potassium level, if still no improvement
- Dextrose 10%, IV, 5 mL/kg over 20 minutes with/without insulin, soluble, 0.1units/kg depending on the blood glucose level.
- if insulin is used -monitor for hypoglycaemia hourly.
- Sodium polystyrene sulphonate, oral/rectal, 1 g/kg in dextrose water.
If hyperkalaemia persists despite above treatment refer the patient urgently for dialysis.
OTHER COMPLICATIONS
Metabolic acidosis: serum pH ≤7.1
- Sodium bicarbonate 4.2 %, IV, 4 mL/kg administered over 2–4 hours.
- Do not mix calcium and sodium bicarbonate containing solutions.
Hypertension
See section Chapter: Cardiovascular System, Hypertension in children .
Infection
Avoid nephrotoxic antibiotics.
Uraemic convulsions
See Chapter: The Nervous System, Seizures .
- Exclude specific causes of convulsions, e.g. hypoglycaemia, hyper- or hyponatraemia, hypocalcaemia or hypertension and treat accordingly.
- Ensure urea levels are appropriately high
- Refer for urgent dialysis
Anaemia
For acute blood loss/active haemolysis and Hb <7 g/dL:
- Packed red cells, IV, 10 mL/kg administered over 6 hours.
Pulmonary oedema, volume overload and hypertension
Do not give fluid to anuric patients with pulmonary oedema.
Intubate and initiate positive pressure ventilation as necessary.
- Furosemide, IV, 2–5 mg/kg administered over 5 minutes.
- Maximum daily dose: 8 mg/kg/24 hours.
- Morphine, IV, 0.1 mg/kg.
- Repeat after 4 hours, if required.
- Oxygen, 100%, 2–3 L/minute by nasal cannula.
Pulmonary oedema is an indication for dialysis in non-responsive cases.
REFERRAL
Urgent for dialysis when:
- Fluid overload is causing pulmonary oedema.
- Anuria >24 hours.
- Central nervous system signs, e.g. convulsions or coma.
- Uraemic bleeding diathesis.
- Uraemic pericarditis.
- Hyperkalaemia or hyponatraemia not responding to conservative treatment.
- Persistent metabolic acidosis pH <7.1 or serum bicarbonate <10 mmol/L.
- Uncontrollable hypertension.
- Severe hyperphosphataemia and hypocalcaemia.