E66
DESCRIPTION
Most children with obesity do not have an underlying pathological cause and have so-called “simple obesity”, i.e. both weight and height are increased.
In children with pathological obesity, the height is not usually increased when compared to parental height. Causes of pathological obesity include syndromes, hypothalamic damage, endocrine abnormalities, immobility, impaired skeletal growth or medicines.
There has been a dramatic increase in the prevalence of childhood overweight and its resultant comorbidities.
DIAGNOSTIC CRITERIA
Clinical
- Measurement of weight alone is inadequate given the influence of height on weight.
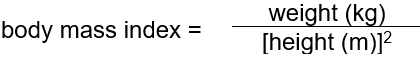
- Assess severity using body mass index (BMI):
- The BMI varies with age. Use sex-specific BMI charts for accurate identification of obesity.
- In general obesity is likely if BMI:
- 19 kg/m² at age 5 years,
- 20 kg/m² at age 10 years, and
- 25 kg/m² at age 18 years.
Investigations
- Fasting glucose and lipid profile.
- ALT, AST, GGT.
GENERAL AND SUPPORTIVE MEASURES
- Weight control by:
- education about the nature of obesity and its long term consequences;
- healthy eating, e.g. regular meal times, avoidance of excessive “snacking”, fried foods, added fats and sugars and high energy drinks while encouraging foods with high fibre content, with modest calorie restriction;
- increasing physical activity;
- reduce sedentary time, e.g. TV watching, computer games, videogames or time on the telephone;
- psychological support, e.g. parental guidance in managing abnormal behaviour.
- Weight loss down to an “ideal body weight for height” is unrealistic. Prevention of further weight gain may produce significant longer-term benefits. If the patient is over 7 years, or if complications are present, aim for a weight loss of 0.5kg/month. Ideally target BMI should be in the overweight range.
MEDICINE TREATMENT
Look for and manage complications such as hyperlipidaemia, hypertension, sleep apnoea, slipped upper femoral epiphysis and non-alcoholic fatty liver. Insulin resistance is another important complication, and this is a key factor in the pathogenesis of metabolic syndrome. Metabolic syndrome is a cluster of cardiovascular and diabetes risk factors such as central abdominal obesity, dyslipidaemia, glucose intolerance, and hypertension (particularly common in patients on HAART).
See Dyslipidaemia and Hypertension in Children ; and 7.5 Diabetes Mellitus.
REFERRAL
- All cases of pathological and morbid simple obesity (as defined by a Z-score>+3).
- Severe/progressive obesity < 2 years.
- Serious co-morbidity requiring weight loss.