T30.0
- Description
- General and supportive measures
- Medicine treatment
- Calculation of initial fluid replacement (after shock has been treated)
- Referral
DESCRIPTION
Burns lead to skin and soft tissue injury and may be caused by:
- heat, e.g. open flame, hot liquids, hot steam;
- chemical compounds;
- physical agents, e.g. electrical/lightning;
- radiation.
GENERAL AND SUPPORTIVE MEASURES
Emergency treatment
- Remove smouldering or hot clothing.
- Remove constrictive clothing/rings.
- To limit the extent of the burn, soak the affected area generously in cold water for not more than 10 minutes.
- In all burns > 10% or where carbon monoxide poisoning is possible (enclosed fire, decreased level of consciousness, disorientation) administer high flow oxygen (15 L/minute).
- Examine carefully to determine the extent and depth of the burn wounds.
- Respiratory obstruction due to thermal injury or soot inhalation, production of black coloured sputum, shortness of breath, hoarse voice and stridor are serious signals and may rapidly proceed to respiratory compromise. Consider early endotracheal airway placement.
Further assessment and care
Assessment:
The extent and depth may vary from superficial (epidermis) to full-thickness burns of the skin and underlying tissues.
Initially, burns are usually sterile.
| Depth of burn wound | Surface/ Colour | Pain sensation/Healing |
|---|---|---|
| Superficial or epidermal | Dry, minor blisters, erythema |
|
| Partial thickness superficial or superficial dermal | Blisters, moist |
|
| Partial thickness deep or deep dermal | Moist white or yellow slough, red mottled |
|
| Full thickness (complete loss of skin) | Dry, charred whitish, brown or black |
|
Burns are classified as minor or major burns.
Major burns:
- Partial thickness burns of > 10% body surface area.
- Full thickness burn of > 3% body surface area.
- Any burn involving the head and face, hands, feet and perineum.
- Inhalation injuries.
- Circumferential burns.
- Electrical burn injuries.
- Burns in neonates.
- Burns in patients with serious pre-existing or concomitant injuries.
Minor burns:
- Partial thickness burns of < 10% body surface area in a child > 1 year of age.
Estimation of burn surface area
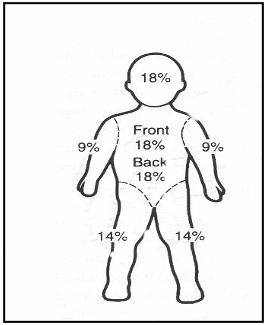
The figure above is used to calculate body surface area %, and indicates percentages for the whole leg/arm/head (and neck in adults) not the front or back.
- In children the palm of the hand is 1%.
- The following adjustments are made in children up to the age of 8 years old after which adult percentages are used for the head, neck and each leg.
- Less than 1 year
- Head and neck are 18% of BSA.
- Each leg is 14% of BSA.
- After the first birthday (> 1 year)
For each year of life: - Head and neck decrease by 1% of BSA until 10% (adult value).
- Leg gains ½ % of BSA until 18% (adult value).
|
Age Years |
Head + neck Front + back |
Torso Front |
Torso Back |
Leg + foot Front + back |
Arm + hand Front + back |
|---|---|---|---|---|---|
| <1 year | 18% | 18% | 18% | 14% | 9% |
| 1 to < 2 years | 17% | 18% | 18% | 14.5% | 9% |
| 2 to < 3 years | 16% | 18% | 18% | 15% | 9% |
| 3 to < 4 years | 15% | 18% | 18% | 15.5% | 9% |
| 4 to < 5 years | 14% | 18% | 18% | 16% | 9% |
| 5 to < 6 years | 13% | 18% | 18% | 16.5% | 9% |
| 6 to < 7 years | 12% | 18% | 18% | 17% | 9% |
| 7 to < 8 years | 11% | 18% | 18% | 17.5% | 9% |
|
8 years and older |
10% | 18% | 18% | 18% | 9% |
Care
Inhalation injury
In addition to other treatment, the degree of inhalation injury may warrant:
- monitoring of blood gases,
- warm humidified oxygen and/or intubation,
- positive pressure ventilation.
Ensure adequate airway in the presence of inhalational burns.
Children with burns may present with delayed onset of airway obstruction. Consider early intubation.
Suspect carbon monoxide poisoning in all fire victims.
- Obtain carboxyhaemoglobin level.
- Treat by administering 100% oxygen.
Prevent heat loss
Nurse all major burns in a warm room (26°C).
Nasogastric drainage
Use a nasogastric tube on free drainage in all burns > 10% (especially during transfer).
After the 1st 24 hours, commence nasogastric feeds in children who had been started on nasogastric drainage where ileus is not suspected.
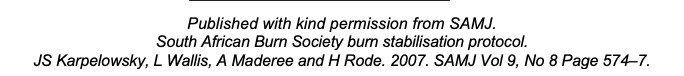
Nutritional support
Consult a dietician as children with burns require a higher than usual intake of nutrients.
Start enteral feeds within 6 hours in burns < 10%.
Estimate daily energy and protein needs using the formulae:
Give iron and vitamins routinely until burn wounds are healed and/or skin grafting has successfully been completed.
Note:
Do not supplement iron during sepsis or infection.
In addition, provide:
- psychological support,
- physiotherapy,
- occupational therapy,
- waterbeds and cradles.
MEDICINE TREATMENT
Fluid replacement
Burns < 10% of total body surface area:
- Oral fluids.
Burns > 10% of total body surface area:
- IV fluid for resuscitation.
If in shock first treat shock. See Shock.
As in all fluid administration in sick children, volumes are estimates and response must be constantly re-evaluated and rates adjusted appropriately.
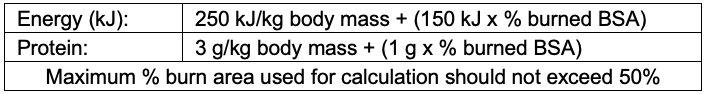
CALCULATION OF INITIAL FLUID REPLACEMENT AFTER SHOCK HAS BEEN TREATED
First 24 hours:
Replacement fluids for burns
- Sodium chloride 0.9%, IV.
- Calculate total fluid requirement in 24 hours:
[Total % burn x weight (kg) x 4 mL] as sodium chloride 0.9%.
Give half of this volume in the 1st 8 hours.
Administer remaining fluid volume in next 16 hours.
- Calculate total fluid requirement in 24 hours:
Note:
If urine output not adequate, increase fluids for the next hour by 50% (continue at higher rate until urine output is adequate then resume normal calculated rate).
PLUS
Maintenance fluids in children
In children, give oral or intravenous maintenance fluid in addition to above calculated volume.
The above are guidelines, need regular review to maintain urine output 1–2 mL/kg/hour.
Avoid circumferential taping when securing infusion lines, as oedema under the eschar may decrease the venous return.
Second 24 hours:
If urine output is adequate, continue resuscitation:
- Sodium chloride 0.9%, IV, 1.5 mL/kg/% burn/ 24 hours.
PLUS
Maintenance:
- ½ Darrows/dextrose 5%, as per maintenance requirement above.
Part of this volume may be replaced by enteral feeds.
Thereafter, progressively decrease IV fluids and increase enteral fluids according to response over time.
Anaemia
If haemoglobin < 7 g/dL:
- Packed red cells, 10 mL/kg over 3 hours.
Hypoalbuminaemia
If indicated by symptomatic hypoalbuminaemia:
- Albumin 20%, IV, 2 g/kg/day. (2 g = 100 mL).
For pain
- Paracetamol, oral, 15 mg/kg/dose 6 hourly as required.
Children with large burns need effective pain relief.
See Management of pain.
Change of dressing
Provide analgesic cover at each dressing change (see Pain Control).
In major burns, change dressings under procedural sedation or general anaesthesia.
Gastric erosions
Preventative medication treatment is not given. Effective early resuscitation and early feeding decrease the incidence of gastric erosion.
If gastric erosion is suspected due to haematemesis or brownish gastric aspirates.
- Omeprazole, oral, 0.4–0.8 mg/kg/dose 12 hourly.
Specialist initiated. - Maximum dose: 20–40 mg/dose.
- If 1 month–2 years: 2.5 mg 12 hourly.
- If > 2–6 years: 5 mg 12 hourly.
- If > 7–12 years: 10 mg 12 hourly.
If unable to take orally:
- Ranitidine, IV, 1 mg/kg 6 hourly.
Local treatment of burns
Gently clean the wounds with running water.
Remove loose skin and debride dead tissue and dress with topical antiseptic cream and non-adherent dressing.
Thereafter, daily rinse with running water and dress with topical antiseptic cream and non-adherent dressing.
In < 20% body surface area burns:
- Povidone-iodine 0.5% with occlusive dressings.
In > 20% body surface area burns:
- Silver-sulphadiazine 1%, on non-adhesive dressings.
- Cover with paraffin gauze.
- Change dressings daily.
Excise and graft all full thickness or deep dermal burns as soon as the patient is stable.
Consider skin grafting in wounds not healed in two weeks.
Antibiotics
Consider if signs of infection are present as these may be subtle:
- pyrexia/hypothermia,
- shock (compensated or not compensated),
- rising pulse or respiratory rate,
- petechiae.
- leucocytosis/thrombocytopaenia,
- looks ill /toxic/altered level of consciousness,
- local inflammatory changes,
The choice of antibiotics is based on the culture and sensitivity results of wound, urine and blood cultures once available.
Positive wound cultures alone do not indicate systemic infections requiring antibiotic treatment.
- Ceftriaxone, IV, 50 mg/kg/dose 24 hourly for 5 days.
If MRSA is suspected or confirmed, replace with:
- Vancomycin, IV, 15 mg/kg/dose 6 hourly for 5–14 days.
AND - Amikacin, IV, for 5–14 days if renal function is satisfactory.
- 1 week to < 10 years: 25 mg stat then 18 mg/kg once daily.
- 10 years and older: 20 mg stat then 15 mg/kg.
Tetanus prevention
Patients with no previous immunisation in the last 5 years:
- Tetanus toxoid, IM, 0.5 mL.
Complete course in previously unvaccinated patients.
Where deep necrotic lesions are part of the burn and if the immunisation status is not known:
- Tetanus immunoglobulin, IM, 500 IU.
Prior to transport/referral
- Commence resuscitative measures, if necessary.
- Administer 100% humidified oxygen by facemask for inhalation injuries, if necessary.
- Cover wounds with clean dressings after hot or smouldering clothing have been removed.
REFERRAL
- Major burn injuries.