I10
HYPERTENSION IN CHILDREN
DESCRIPTION
Hypertension is defined as systolic and/or diastolic blood pressure ≥ the 95th percentile for gender, age and height percentile on at least three consecutive occasions. A sustained blood pressure of >115/80 mmHg is abnormal in children between 6 weeks and 6 years of age. Measure blood pressure with the child in a sitting or supine position with the entire arm in line with the level of the heart.
In children, it is easier to monitor the systolic blood pressure because of better correlation and less technical pitfalls than diastolic blood pressure.
In the majority of children, hypertension is due to an identifiable cause. Severe hypertension suggests renal disease.
Hypertensive emergency/crisis exists when CNS signs of hypertension appear such as encephalopathy, convulsions, retinal haemorrhages or blindness. Great care is required to reduce the blood pressure in a controlled manner to avoid potentially serious consequences of impaired auto-regulation of cerebral blood flow.
Hypertensive urgency is defined as a significant elevation of blood pressure without accompanying end organ damage. Patients are generally symptomatic with complaints of headache, blurred vision and nausea, despite the lack of end organ involvement.
A valid assessment of the blood pressure is of extreme importance. The blood pressure is measured by standard auscultation technique in children > 1 year of age.
In children < 1 year of age, a flush technique is usually used, although Doppler measurement would be preferable.
Measure the BP in at least one limb, preferably the right upper arm. If hypertension is present, measure BP on all four limbs.
One should use the widest cuff that can be applied to the upper arm. The cuff bladder must encircle at least 80% of the upper arm and should cover at least 75% of the distance between the acromion and the olecranon. It is better to use a cuff that is slightly too large than one that is too small. Large cuffs, if covered with linen-like material, can be folded to the appropriate size in smaller infants as long as the bladder encompasses the arm.
DIAGNOSTIC CRITERIA
Clinical
- Symptoms and signs of any of the following systems:
- central nervous,
- cardiovascular,
- respiratory,
- urogenital.
- The most common associated features are:
- oedema, haematuria, proteinuria,
- skin sores (impetigo),
- convulsions, coma and visual symptoms,
- acute heart failure and pulmonary oedema,
- acute respiratory distress, cyanosis and apnoea.
- Some children may be asymptomatic.
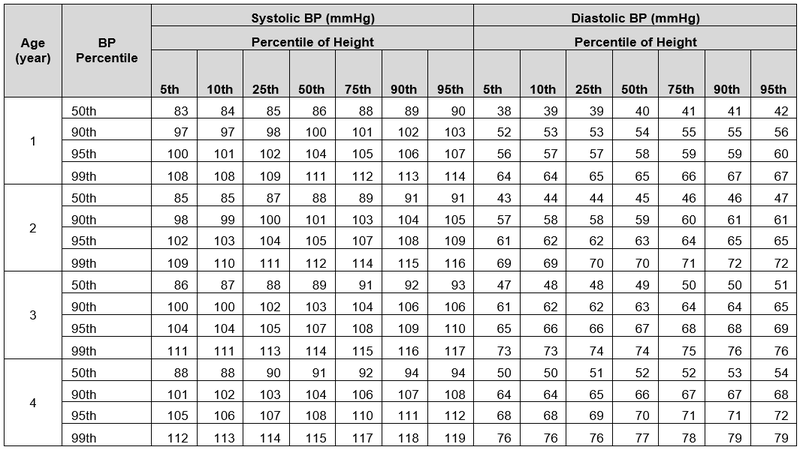
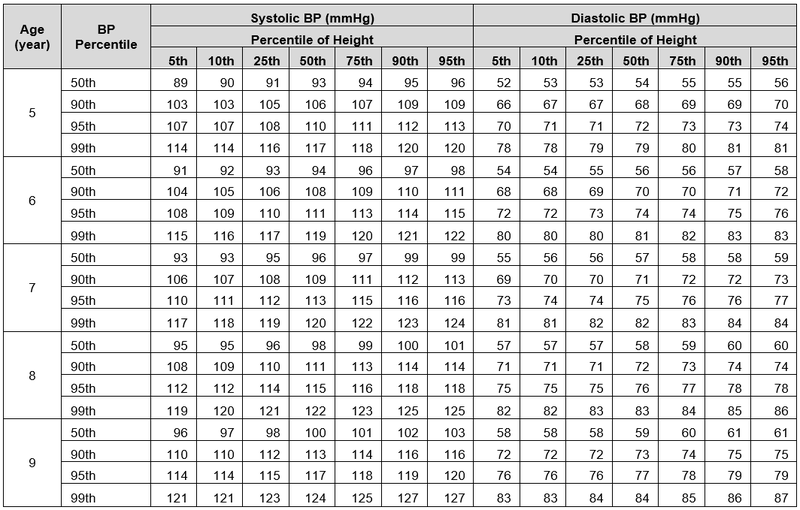
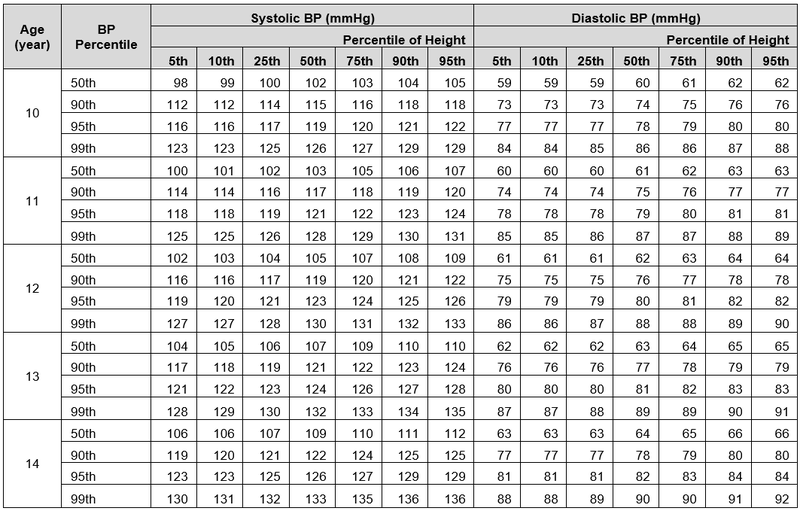
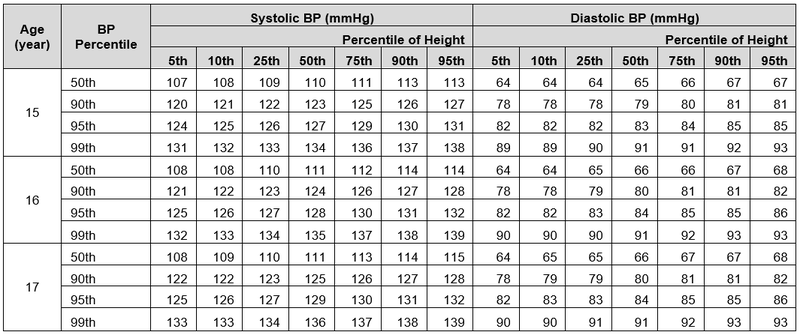
- Blood pressure in children correlates with body size and increases with age.
Categories of hypertension
- Normal: below 90th percentile.
- Prehypertension: 90th –95th percentile or BP > 120/80 mmHg.
- Stage 1 hypertension: > 95th –99th percentile plus 5 mmHg.
- Stage 2 hypertension: > 99th percentile plus 5 mmHg.
| Age of child |
95 th Percentile of systolic and diastolic blood pressure |
|
|---|---|---|
| First 12 hours | First week | |
| newborn premature | 65/45 mmHg | 80/50 mmHg |
| newborn fullterm | 80/50 mmHg | 100/70 mmHg |
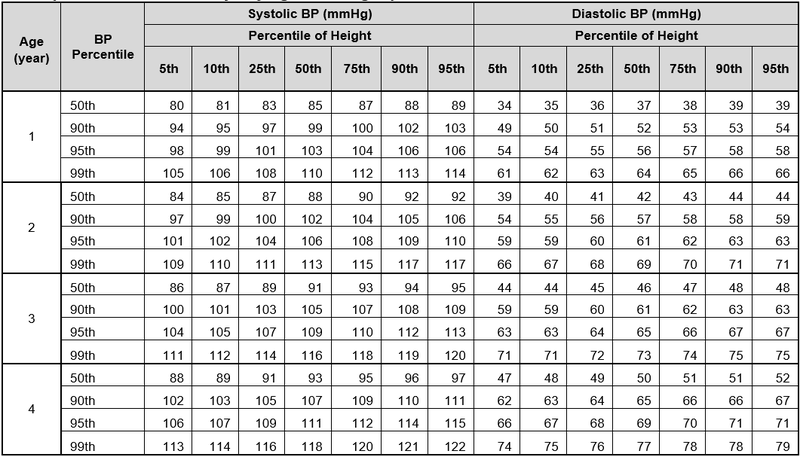
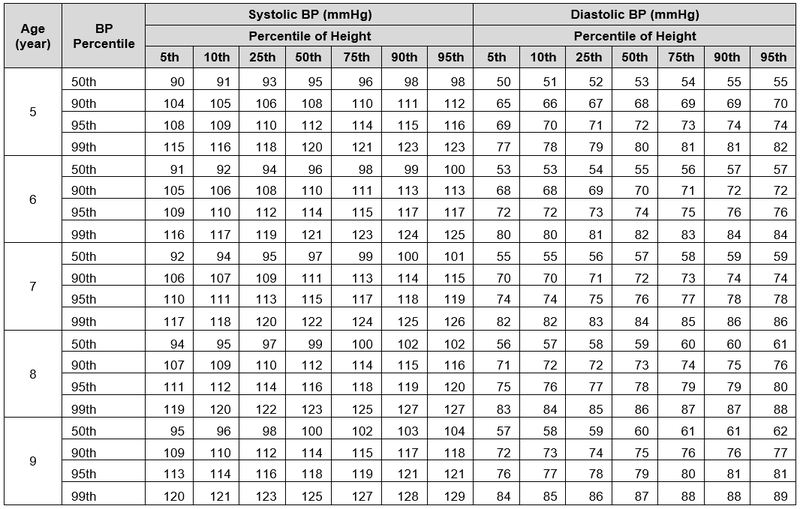
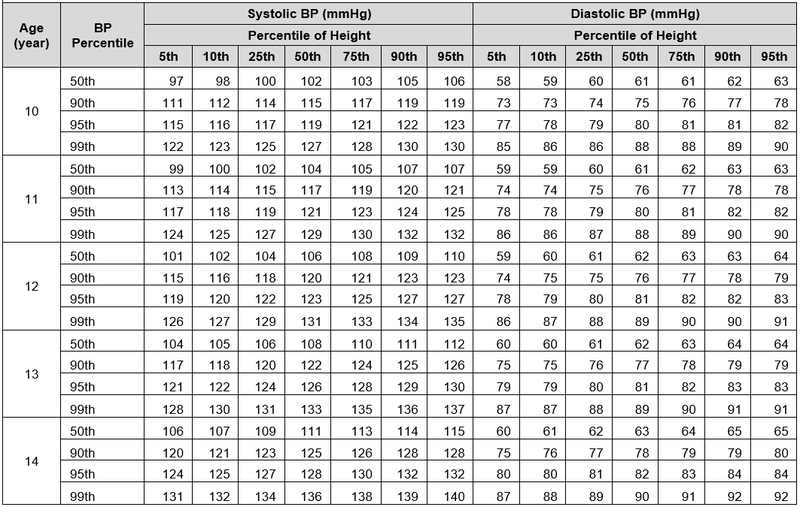
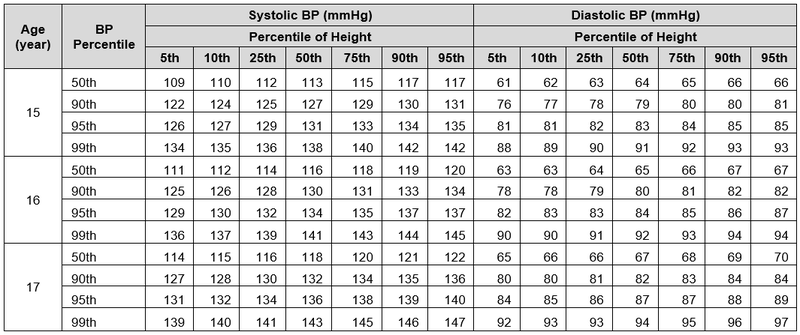
Blood pressure levels for Boys by age and height percentile
Blood pressure levels for Girls by age and height percentile
GENERAL AND SUPPORTIVE MEASURES
- There is a strong association between overweight patients and high blood pressure.
- The majority of these patients have mild hypertension and usually only need lifestyle modification.
- Acute hypertension:
- Bed rest – fowler’s position.
- Control fluid intake and output (restriction).
- Restrict dietary sodium.
- Manage end organ effects.
- Chronic hypertension:
- Advise a change in lifestyle.
- Institute and monitor a weight reduction programme for obese individuals.
- Regular aerobic exercise is recommended in essential hypertension.
- Dietary advice:
- Limit salt and saturated fat intake.
- Increase dietary fibre intake.
HYPERTENSION, ACUTE SEVERE
I10
For acute or chronic hypertension, blood pressure needs to be lowered cautiously.
Initiate medicines for sustained control as soon as possible to maintain the effect when the emergency measures are discontinued.
Rate of BP reduction depends upon starting BP and age of the child.
In the absence of central nervous system signs, acute hypertension can be rapidly controlled over 24 hours. If in doubt about the duration of hypertension, reduce BP slower over 48 hours.
Aim to reduce the systolic BP with not more than ⅓ of the interval between the patient’s systolic blood pressure and the 95th percentile for that age or height in the first 8 hours, then a further gradual decline over the next 24–48 hours.
Do not decrease BP to < 95th percentile in first 24 hours.
GENERAL AND SUPPORTIVE MEASURES
- Admit patient to paediatric intensive care unit, if possible.
- Monitor BP every 10 minutes until stable, thereafter every 30 minutes for 24 hours.
- Set up two peripheral intravenous drips.
MEDICINE TREATMENT
Do not combine medicines of the same class.
- Furosemide, IV, 1–2 mg/kg as a bolus slowly over 5 minutes.
- If oliguric, maximum dose: 5 mg/kg/dose.
- Repeat appropriately for fluid overload.
AND
- Labetalol, IV, 0.5–3 mg/kg/hour.
- 100 mg labetalol in 80 mL sodium chloride 0.45% = 1 mg/mL.
- Infuse with infusion pump.
- Give bolus of 0.5 mg/kg and then titrate the dose slowly upwards until the desired blood pressure is achieved.
- Repeat based on BP response.
If there is an inadequate response:
ADD
- Amlodipine, oral, 0.2 mg/kg/dose.
- May be repeated after 12 hours.
- Thereafter every 24 hours.
If phaeochromocytoma suspected use an alpha blocker instead of amlodipine while tapering labetalol, e.g.:
- Prazosin, oral, 12 hourly.
- 1 month to 18 years: 0.005 mg/kg as a test dose, then 0.025-0.1mg/kg adjusted according to response.
In patients with hypertension due to a neurosecretory tumour (phaeochromocytoma or neuroblastoma), use an α-blocker either as single medicine or in combination with β-adrenergic blocker.
Once blood pressure is controlled, taper to oral treatment.
See section Hypertension, chronic.
URGENT REFERRAL
- Severe hypertension for specific diagnosis and treatment.
HYPERTENSION, CHRONIC
I10
DESCRIPTION
Primary/Essential hypertension
Occurs most commonly in adolescents.
The patient is often asymptomatic and well.
It is diagnosed by excluding underlying causes of hypertension.
Hypertension is confirmed by sustained high blood pressure measured on 3 follow-up occasions.
Chronic secondary hypertension
All children with incurable forms of persistent secondary hypertension require medicine treatment over and above general and supportive measures.
DIAGNOSTIC CRITERIA
Investigations
- Urine dipstick test.
- Urine MCS.
- Blood urea, calcium, creatinine and electrolytes.
- Chest X-ray, ECG and abdominal ultrasound.
If all tests are negative, start lifestyle intervention.
GENERAL AND SUPPORTIVE MEASURES
- Introduce physical activity, diet management and weight reduction, if obese.
- Advise teenagers against smoking.
- Follow up to monitor blood pressure and educate patient on hypertension:
- if blood pressure decreases, continue with non-drug management and follow up;
- if BP is increasing progressively, reinvestigate to exclude secondary causes or refer;
- if BP is stable but persistently > 95th percentile and secondary causes have been excluded, start medicine treatment after failed non-drug management for 6 months.
- Consider earlier initiation of medicine treatment if positive family history for cardiovascular disease, essential hypertension or diabetes mellitus.
MEDICINE TREATMENT
Goal of treatment in uncomplicated primary hypertension with no target-organ damage is to achieve BP < 95th percentile. For chronic renal disease, diabetes or hypertension with target-organ damage, target is BP < 90th percentile.
Medicine treatment is initiated for Stage 2 hypertension. Consider therapy in Stage 1 hypertension if there is a family history of cardiovascular disease, hypertension or diabetes.
Aim to achieve control of BP over 48–72 hours in symptomatic patients.
For ambulatory patients start at the lowest dose of the preferred medicine and increase the dose until control is achieved.
Once the highest recommended dose is reached or if the patient experiences adverse effects from the medicine, add a second medicine from a different class.
For patients with persistent hypertension despite the use of first line medicine, add a second/third medicine. There is no specific order in which medicine should be added.
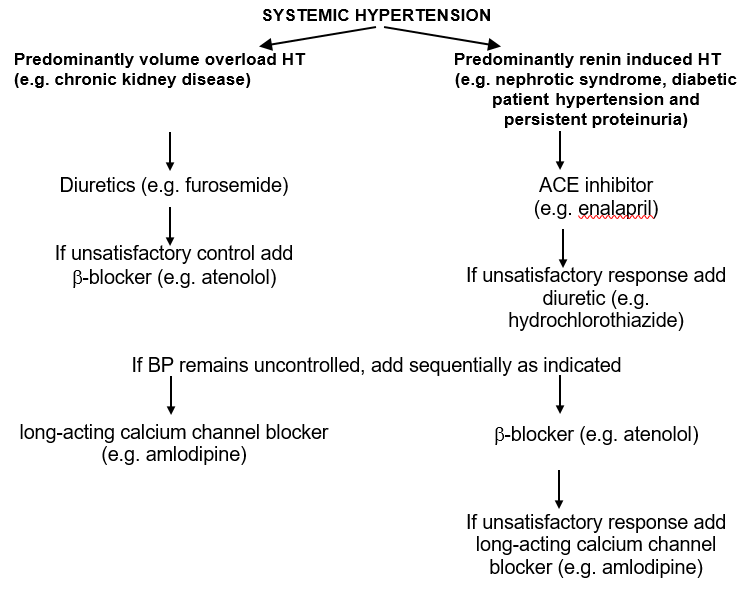
Use specific classes of antihypertensive medicine according to the underlying pathogenesis or illness.
ACE inhibitor
Contraindicated in bilateral renal artery stenosis.
- Enalapril, oral, 0.04 mg/kg/dose 12 hourly.
- Maximum 0.3 mg/kg/dose up to 40 mg/day.
OR
For young children less than 10 kg body weight:
- Captopril, oral.
- Initial dose: 0.1 mg/kg/dose 8 hourly.
- Maximum 2 mg/kg/dose.
β-blocker
- Atenolol, oral, 0.5–1 mg/kg/dose once daily.
- Maximum dose: 2 mg/kg/day.
- Contraindicated in severe heart failure and asthma.
OR
If child less than 10 kg body weight:
- Propranolol, oral, 0.25–1 mg/kg/dose 8–12 hourly.
- Maximum dose: 1.5 mg/kg/dose.
Calcium channel blocker
- Amlodipine, oral, 0.1–0.2 mg/kg/dose once daily.
Diuretic
- Hydrochlorothiazide, oral, 0.5–1 mg/kg/dose once daily.
- May cause hypokalaemia.
OR
- Furosemide, oral, 0.5–1.5 mg/kg/dose 12–24 hourly.
- Maximum dose: 6 mg/kg/day.
- May cause hypokalaemia.
α-blocker,
Also indicated in patients with phaeochromocytoma-associated hypertension.
- Prazosin, oral, 12 hourly.
- 1 month to 18 years: 0.005 mg/kg as a test dose, then 0.025-0.1mg/kg adjusted according to response.
REFERRAL
- All children with chronic hypertension for specific diagnosis, planning of treatment and long-term follow-up.