I49.9
- Description
- Diagnostic criteria
- Tachydysrhythmia
- Bradydysrhythmia
- General and supportive measures
- Medicine treatment
- Referral
DESCRIPTION
A heart rate that is either abnormally slow or fast for age or irregular.
Normal heart rate/minute for age:
Newborn 100–160
< 1 year 110–160
1–2 years 100–150
2–5 years 95–140
5–12 years 80–120
> 12 years 60–100
DIAGNOSTIC CRITERIA
Clinical
- Presenting features may vary with the age of the patient:
- infants:
- colour changes (pale, mottled),
- irregular pulse,
- irritability,
- tachycardia,
- feeding difficulties,
- bradycardia,
- sweating,
- signs of cardiac failure,
- tachypnoeic/apnoeic spells.
- children:
- dizziness,
- tachycardia,
- palpitations,
- bradycardia,
- fatigue,
- syncope,
- chest pain,
- signs of cardiac failure.
Investigations
- ECG is essential for diagnosis, preferably a 12- lead ECG.
- Monitors are inadequate to diagnose most dysrhythmias.
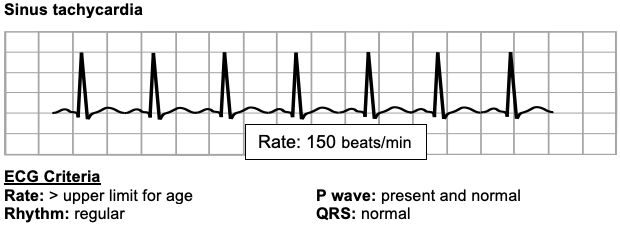
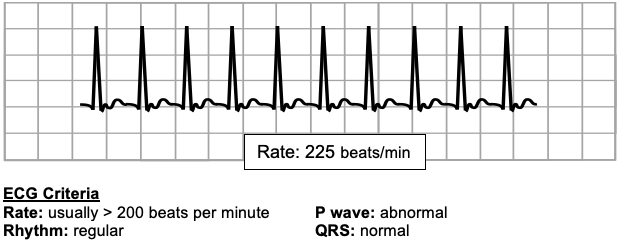
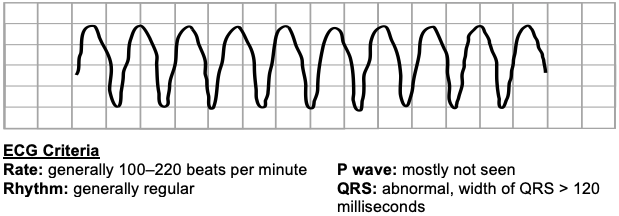
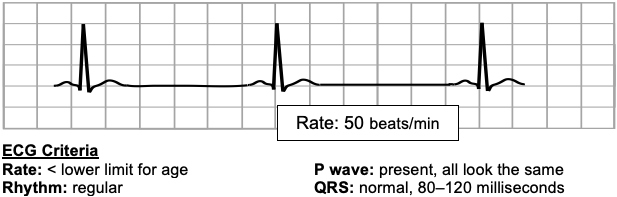
- A standard ECG is recorded at 25mm/second. Each small block on the ECG paper is 1mm x 1mm and represents 40 milliseconds and each large block 5mm x 5mm and represents 200 milliseconds. A length of 300 large blocks represents 1 minute and the heart rate can be estimated from the ECG strip by dividing 300 by the number of large blocks between sequential R waves provided that there is not substantial variability in the RR interval lengths. The ECG tracings below show only the large (5mm) blocks.
TACHYDYSRHYTHMIA
Sinus tachycardia
Supraventricular tachycardia
Ventricular tachycardia
BRADYDYSRHYTHMIA
Important causes of bradycardia:
Hypoxia
Drug ingestion
Congenital heart block
Excessive vagal stimulation
Sinus bradycardia
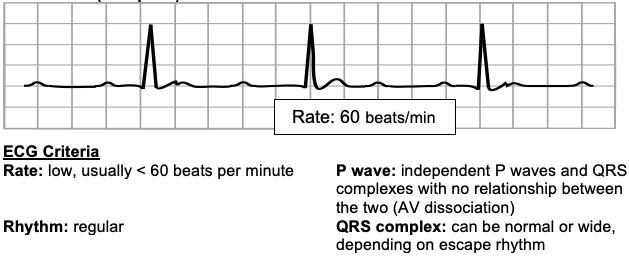
Heart block (Complete)
GENERAL AND SUPPORTIVE MEASURES
- Sinus tachycardia usually requires management of the underlying condition.
- Apply ABC of resuscitation if needed.
- Admit to high care or intensive care unit if indicated.
- Monitor:
- ECG,
- oxygen saturation,
- blood pressure,
- haemoglobin,
- heart rate,
- acid–base status,
- respiratory rate,
- blood gases.
- Maintain adequate nutrition and hydration.
- Treat pyrexia.
MEDICINE TREATMENT
Tachydysrhythmia
Emergency treatment.
Narrow complex tachycardia
Commonly due to supraventricular tachycardia.
Stable patient:
Attempt vagal stimulation.
- Place ice bag on face, or
- Infants: immerse face in ice-cold water for a few seconds.
- Older children: try a valsalva manoeuvre.
- Eye-ball pressure and carotid massage is contraindicated in children.
- In consultation with a paediatric specialist: Adenosine, IV, 0.1 mg/kg rapid IV push (within seconds).
- Follow immediately with a rapid flush of at least 5 mL sodium chloride 0.9%.
- Increase dose in 0.1 mg/kg increments every 2 minutes until return of sinus rhythm. Follow each dose with a rapid flush of sodium chloride 0.9%.
- Maximum dose: 0.5 mg/kg. Do not exceed 12 mg in total.
- Because adenosine is rapidly metabolised, inject adenosine into an intravenous cannula capable of supporting rapid infusion and preferably located as centrally as possible (i.e. cubital rather than hand or foot). Follow immediately, with a rapid flush of a fluid bolus. It is helpful to have both the syringe with adenosine and the fluid bolus connected to the giving set. The line between the syringes and the patient should be as short as possible.
Unstable patient – heart failure / shocked:
DC synchronised cardioversion at 1- and then 2 J/kg.
If possible, empty the stomach before cardioversion is attempted. Resuscitation facilities must be available.
Midazolam for sedation, if necessary.
Broad complex tachycardia
Commonly due to ventricular tachycardia.
Causes include electrolyte disturbances and drug ingestion.
Stable patient (rare):
- Send ECG immediately to paediatric cardiologist.
- AVOID giving adenosine to patients with broad complex tachycardia unless the rhythm is regular with a monomorphic QRS complex
Medicines that may be recommended by a paediatric cardiologist include:
- Magnesium sulphate intravenous 25-50 mg/kg over a few minutes for torsade de pointes.
- Amiodarone intravenous 5mg/kg over 20 minutes.
Unstable patient – heart failure/shock:
- Pulseless treat as ventricular fibrillation. See Cardiorespiratory arrest
- DC synchronised cardioversion at 1- and then 2 J/kg.
- If synchronised cardioversion fails, use asynchronised shocks.
- Resuscitation facilities must be available.
- Midazolam for sedation, if level of awareness indicates.
Monitor and correct electrolytes and acid-base status on blood gases. Consider underlying causes.
If DC cardioversion fails:
- Amiodarone, IV, 5 mg/kg slowly over 20 minutes.
And continue with DC cardioversion.
BRADYDYSRHYTHMIA
Try and correct underlying causes.
Stable patient:
Observe.
Bradydysrhythmia due to vagal stimulation:
- Atropine, IV/IO, 0.02 mg/kg. Maximum single dose 0.5mg.
- If no response, repeat in 5 minutes.
Unstable patient:
Treat as impending arrest:
- Adrenaline (epinephrine), IV/IO, 0.01 mg/kg.
- Repeat if necessary conferring with referral institution.
If no sustained response, consider:
- Adrenaline (epinephrine), IV infusion, 0.05–2 mcg/kg/minute.
REFERRAL
- All children with tachydysrhythmias after acute treatment, excluding sinus tachycardia due to other causes.
- Bradycardia unresponsive to medical treatment, or heart block.