E40–E46
MALNUTRITION, SEVERE ACUTE
E40–E43
Z-scores
- For practical purposes a “z-score” is the number of standard deviations (SD) below or above the mean.
- 2 SD or 2 z-scores above the mean (+2) equates fairly closely to the 97th percentile and 2 SD or 2 z-scores below the mean (–2) equates fairly closely to the 3rd percentile.
- 3 SD or 3 z-scores above or below the mean would be regarded as severe deviation from normal.
- In deviation below normal, consider if a reasonable explanation exists, e.g. severe low birth weight with adequate growth profile subsequently.
Admit all cases with complicated severe acute malnutrition.
Uncomplicated cases may be managed with “ready to use therapeutic food (RUTF)” in ambulatory setting where this service is established.
DESCRIPTION
Severe Acute Malnutrition (SAM)
A multi-deficiency state of severe undernutrition of essential nutrients exacerbated by acute/chronic infection and metabolic disturbances. Severe Acute Malnutrition (SAM) includes but is not restricted to the clinical entities of bilateral pitting oedema or severe wasting. It is associated with a high but significantly modifiable mortality.
Criteria for ambulatory treatment of severe acute malnutrition,
All of the following must apply:
- Children over the age of 6 months with no pitting oedema.
PLUS - Alert and feeding well.
PLUS - None of the IMCI danger signs/nor those listed below.
PLUS - Exclusion of other morbidity, TB and HIV infection.
DIAGNOSTIC CRITERIA
SAM in children aged 6–60 months:
| Indicator | Measure | Cut-off |
|---|---|---|
| Severe wasting | Weight-for-height | z–score less than –3 |
| Severe wasting |
Mid upper arm circumference (MUAC) |
Less than 11.5 cm |
| Bilateral pedal oedema | Clinical sign |
Where a suitable measuring device is not available the following less sensitive findings would also indicate the need to manage as severe acute malnutrition:
- Severe underweight
- weight for age z-score less than –3 (usually clinically reflective of marasmus) where no other reasonable explanation is present, and/or
- clinically visible severe wasting (usually clinically reflective of marasmus – thin arms, thin legs, “old man” appearance, baggy pants folds around buttocks, wasted buttocks).
- Nutritional oedema (usually clinically reflective of kwashiorkor – bilateral pedal oedema usually supported by findings of skin changes, fine pale sparse hair, enlarged smooth soft liver, moon face).
Danger signs:
- Lethargy.
- Hypoglycaemia.
- Shock.
- Jaundice.
- Refusing feeds.
- Dehydration.
- Weeping skin lesions.
- Respiratory distress.
- Hypothermia.
- Convulsions.
- Bleeding.
- Vomiting everything.
Note: Any of these danger signs indicates the need for more intensive inpatient management.
Time frame for inpatient management of severe acute malnutrition
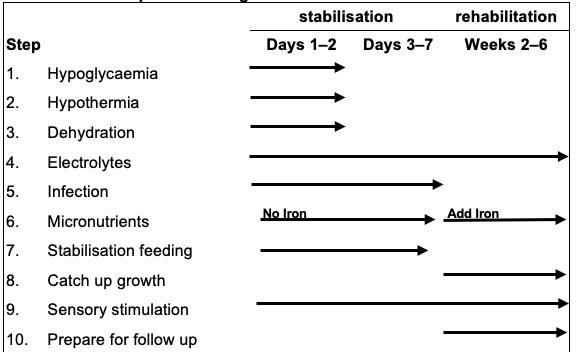
The general approach to the inpatient management of severe acute malnutrition is encapsulated in the 10 step approach illustrated above.
Within this approach the first days are involved in achieving metabolic and physical stability and this phase usually moves to the rehabilitation phase somewhere between the 3rd and 7th day of admission.
Stabilisation phase:
- feeding,
- preventing/treating hypoglycaemia,
- preventing/treating hypothermia,
- treating infections,
- giving minerals, vitamins and trace elements, and
- preventing/treating dehydration.
Rehabilitation phase:
- continued feeding,
- catch up growth,
- management chronic infections/infestations,
- continued administration of minerals and vitamins (including commencing iron),
- play and love; stimulation, and
- preparation for discharge.
Step 1: Hypoglycaemia (Blood glucose <3 mmol/L)
Prevention
Feed child with severe acute malnutrition immediately (within 30 minutes of presentation) and then ensure every feed is given by day and at night. See step 7: Stabilisation feeding.
Keep the child warm. See step 2: Hypothermia.
Detection and treatment
Test blood glucose level 3 hourly in severely ill child for first 24 hours and until stable (longer if the child is very ill).
Asymptomatic hypoglycaemia:
If blood glucose < 3 mmol/L in asymptomatic child, give immediately (oral bolus):
- Stabilisation/F75 formula, oral, 15 mL/kg.
OR
- Dextrose, 10%, oral, 10 mL/kg.
- Dextrose 10% = Dextrose 50% 2 mL/kg with water for injection 8 mL//kg.
OR
- Sugar solution, oral, 10 mL/kg
- 1 rounded teaspoon sugar in 50 mL or 3 ½ tablespoons of water.
Check blood glucose after 30 minutes and maintain it above 3 mmol/L. Continue feeds.
If symptomatic or persistent hypoglycaemia:
- Dextrose, 10%, IV, 5 mL/kg.
OR
- Neonatal maintenance solution, IV, 5 mL/kg.
Continue feeds once responsive.
- Change feeds to 2 hourly if hypoglycaemia has occurred. See step 7: Stabilisation feeds.
These children have poor cardiac reserves and are easily volume overloaded. Do not start or maintain IV infusions unless absolutely necessary.
Step 2: Hypothermia (Axillary temperature <35ºC)
Prevent hypothermia
Care for child in a warm area, i.e. 25–30ºC room temperature.
Ensure child’s body, especially the head, is covered at all times particularly at night.
Avoid drafts and change wet napkins/clothing.
Avoid exposure e.g. bathing.
Feed immediately and 2–3 hourly as this provides energy to generate heat.
Allow child to sleep with mother/carer at night for warmth.
Treat hypothermia
Check axillary (underarm) temperature, 3 hourly.
Axillary temperature <36ºC indicates an urgent need to warm child.
Allow child to sleep with mother/carer at night for warmth. Use mother-child skin-skin contact, i.e. Kangaroo care, to keep child warm and wrap both with blankets.
Place heater nearby. If a radiant heater is used for warming check temperature at least every ½ hour.
If severely hypothermic and not improving use other heating measures but do not apply direct heat to the skin as this may burn the child.
Check temperature 2-hourly until > 36.5ºC. Consider and treat for infection and sepsis. See step 5: Infection.
Step 3: Dehydration
See Diarrhoea, acute.
Continue feeds and other care of severe malnutrition.
Step 4: Electrolytes (hypokalaemia, hypomagnesaemia, hypophosphataemia and hypernatraemia)
All severely malnourished children have excess body sodium even though the plasma sodium may be low. Oedema is partly due to these imbalances, not fluid overload.
Giving high sodium load fluids is dangerous.
Do NOT treat oedema with a diuretic.
Potassium
Serum potassium does not indicate total body potassium status. Potassium supplementation is required unless frank hyperkalaemia.
Feeds made with combined mineral and vitamin complex contains potassium. When this is used, do not add further potassium.
If the formula is made without combined mineral and vitamin complex, add potassium:
- Potassium chloride solution, 25–50 mg/kg/dose, oral, 8 hourly until oedema subsides:
- If < 10 kg: 250 mg.
- If > 10 kg: 500 mg.
Magnesium
Feeds made with combined mineral and vitamin complex or trace element mix contains magnesium. If formula is made without either of these additives, add magnesium:
- Trace element mix, oral, daily.
- If < 10 kg: 2.5 mL.
- If > 10 kg: 5 mL.
OR - Magnesium sulphate 50%, oral, 0.2 mL/kg as a once daily dose for at least 2 weeks. The IV preparation can be given orally.
Refeeding syndrome may occur at any stage during the stabilisation phase. Regular phosphate level monitoring is advisable and cautious feeding with slow feed advancement is encouraged.
Phosphate replacement:
If serum phosphate 0.73–0.96 mmol/L give 0.32 mmol (0.25 ml/kg) in divided dosages orally.
If serum phosphate 0.51–0.72 mmol/L give 0.64 mmol/kg (0.5 ml/kg) in divided dosages orally.
- If serum phosphate less than 0.5 mmol/L give 1.0 mmol/kg (0.75 ml/kg) in divided dosages orally.
Phosphate enemas have 1.38 mmol/ml phosphate.
Step 5: Infection
Antibiotics
Start antibiotics on the first day at admission.
If the child has no danger signs, is alert and feeding well:
- Amoxicillin, oral, 30 mg/kg/dose 8 hourly for 5 days.
All other children:
- Ampicillin, IV/IM, 50 mg/kg 6 hourly for 7 days.
- Avoid IV infusions, if possible. Use a heparin lock to avoid fluid overload because of poor cardiac reserves.
PLUS
- Avoid IV infusions, if possible. Use a heparin lock to avoid fluid overload because of poor cardiac reserves.
- Gentamicin, IV, 6 mg/kg once daily for 7 days.
As soon as there is a response and patient can tolerate oral medication change ampicillin to amoxicillin and continue with gentamicin:
- Amoxicillin, oral, 30 mg/kg/dose 8 hourly for a further 5 days.
PLUS - Gentamicin, IV/IM, 6 mg/kg once daily for 7 days.
If the child is severely ill or fails to improve after 48 hours:
- Third generation cephalosporin, e.g.:
- Ceftriaxone, IV/IM, 50 mg/kg/dose once daily.
- If meningitis suspected: use 80 mg/kg/dose.
- Ceftriaxone, IV/IM, 50 mg/kg/dose once daily.
If child does not improve after 5 days, or deteriorates:
- Refer to higher level of care.
Intestinal worm infestation
Treat after the acute phase:
Children 1–2 years of age:
- Mebendazole, oral, 100 mg 12 hourly for three days.
Children > 2 years:
- Mebendazole, oral, 500 mg as a single dose immediately.
HIV and TB
In children with HIV and TB, good recovery from malnutrition is possible but may take longer. Treatment failure of malnutrition may be more common.
Actively investigate for TB and HIV as soon as possible.
TB is difficult to diagnose and confirm.
Ask about contacts, symptoms, do tuberculin skin test (TST) and chest X-ray. If TST negative, repeat just before discharge.
If TB is clinically likely, presumptive TB treatment is often reasonable, but once begun should be completed. See Chapter - Tuberculosis, Tuberculosis, pulmonary.
HIV is relatively simple to diagnose and confirm.
Children < 18 months: PCR and confirm with viral load > 10 000 copies/mL.
Children ≥ 18 months: rapid test/ELISA and confirm with different rapid test/ELISA.
ART is the same as for HIV negative children.
Once the child enters the rehabilitative phase, commence antiretroviral therapy without delay if HIV infected. See Chapter – Human Immunodeficiency Virus Infection, Human immunodeficiency virus infections.
Step 6: Micronutrients
Vitamins
- Vitamin A, oral, as a single dose:
| Age | Dose | No. of capsules |
|---|---|---|
| Infants < 6 months: | 50 000 IU | 1 capsule |
| Infants 6–11 months: | 100 000 IU | 1 capsule |
| Children 12 months to 5 years: | 200 000 IU | 1 capsule |
Record doses in the Road-to-Health booklet.
All children with clinical signs of severe vitamin A deficiency (eye changes: xerophthalmia, corneal ulceration, Bitot's spots, corneal clouding) and severe measles:
- Vitamin A, oral, 3 doses.
- First dose, immediately; second dose on day 2 and third dose after 14 days.
- Record the dose given in prescription and the Road to Health Book.
If on feeds with combined mineral and vitamin complex:
- Folic acid, oral, 2.5 mg as a single dose.
If not on feeds with combined mineral and vitamin complex:
- Folic acid, oral, 2.5 mg as a single daily dose.
PLUS - Multivitamin, oral, 5 mL as a single daily dose.
Anaemia in malnourished children
Non-acute management:
Although anaemia is common, do NOT give iron initially but wait until the child has a good appetite and starts gaining weight (usually by the second week).
Treat severe anaemia with blood transfusion, if:
- Symptomatic anaemia (Hb usually below 4 g/dL).
OR - If there is respiratory distress with a low Hb.
- Packed red cells, IV, 5 mL/kg administered over 3 hours.
PLUS - Furosemide, IV, 1 mg/kg at the start of the transfusion.
Repeat only if severe anaemia or respiratory distress persists and the haemoglobin is still low.
Once gaining weight and oedema has resolved:
- Iron, oral, 2 mg/kg elemental iron per dose 8 hourly with meals.
- Continue for at least 2 months to replace iron stores.
Step 7: Stabilisation feeding
Immediate: stabilisation phase:
Begin feeding immediately – do not miss feeds.
Give “F75/stabilising feed” at 130 mL/kg/day divided into 3 hourly feeds, i.e. 8 times daily. Give all feeds including that at 03h00.
If child has gross oedema i.e. if the oedema is up to or beyond the knee or anasarca, give 100 mL/kg initially and increase progressively.
Monitor and record intake carefully.
| F75 formula/Stabilisation | |
|---|---|
| Fresh cow’s milk | 300 mL |
| Sugar | 100 g |
| Vegetable oil | 20 g |
| Combined mineral and vitamin complex* | indicated by insert |
| Water to make up to: | 1 000 mL |
*If no combined mineral and vitamin complex:
- Trace element mix, oral, 20 mL daily.
If danger signs, hypothermia or hypoglycaemia present, feed the same daily volume but divided into 2 hourly feeds, i.e. 12 times daily. Give all feeds including those at 02h00 and 04h00.
Give from a cup. Very weak children may be fed by spoon, dropper or syringe.
If feeds refused/not finished (i.e. less than 80% of daily amount taken) give all feeds via nasogastric tube.
Weigh daily and plot weight gain.
Readiness to enter the rehabilitation phase is signalled by a return of appetite, usually about one week after admission.
Step 8: Transition feeding and catch up growth
Feeding (rehabilitation phase)
- Transition
- For the first two days replace the initial feeds with equal amounts of “rebuilding/catch-up/F100 formula”. Gradually increase the volume by 10 mL/feed until some formula remains unfinished, usually ± 200 mL/kg/day.
- When appetite returns introduce a modified diet. Balance the intake by giving 3 modified meals and 5 feeds of F100. Prepare food without adding salt.
| F75 formula/Stabilisation | |
|---|---|
| Fresh cow’s milk | 880 mL |
| Sugar | 75 g |
| Vegetable oil | 20 mL |
| Combined mineral and vitamin complex* | as indicated by insert |
| Water to make up to: | 1 000 mL |
*If no combined mineral and vitamin complex:
- Trace element mix, oral, 20 mL.
Monitor progress after the transition by assessing the rate of weight gain.
Weigh child each morning before feeding and plot the weight.
Each week calculate and record weight gain as g/kg/day.
If weight gain is:
- poor (< 5 g/kg/day) – child requires full reassessment.
- moderate (5–10 g/kg/day) – check whether intake targets are being met, or if infection has been overlooked.
- good (>10 g/kg/day) – continue to praise staff and mothers.
Step 9: Sensory stimulation
Stimulation and loving care
- Provide tender loving care.
- Help and encourage mothers to comfort, feed and play with their children.
- Involve occupational therapist, if available, for structured play otherwise arrange this as best possible in the ward.
- Provide a stimulation program in the ward.
Step 10: Prepare for follow up
Preparation for discharge
- Obtain information on household food security, family background and socio-economic status and refer appropriately.
- Instruct mothers how to modify family foods, how often to feed, what and how much to give.
- Ready to Use Therapeutic Foods (RUTF) may be supplied to facilitate earlier discharge where this is indicated and available.
- Involve mother in discharge planning and follow up plans.
- Social assessment: Before discharge, ensure parent/caregiver is able to access food for the child, ensure all financial supports and grants have been accessed. A social worker may assist in ensuring this. The social worker should also assess for other social risks.
- Make follow-up arrangements. Link patient to PHC systems and Family Health Teams/Community Care Givers Workers for close follow-up and monitoring of feeding and compliance with therapeutic feeding program.
- Ensure all immunisations are up to date.
- Do not discharge any malnourished child without having adequately investigated for TB and HIV infection. Repeat TST before discharge as immunity may have returned to normal.
- Write full clinical summary in Road to Health book.
Discharge criteria
- good appetite,
- no infection,
- no oedema,
- continuous good weight gain for last 5 days,
- playful and alert, and
- all preparation in place for discharge.
Feed volume charts
Initial stabilisation /F75 formula volumes at 130 mL/kg/day.
Use 2 hourly if child very sick or has hypoglycaemia or hypothermia.
|
Childs Weight (kilograms) |
Amount feed | Amount feed |
If total volume taken in a day is less than the below figure change to nasogastric feeding |
|---|---|---|---|
|
Every 3 hours 8 times a day |
Every 2 hours 12 times a day |
||
| 2 | 35 | 25 | 210 |
| 2.1 | 35 | 25 | 220 |
| 2.2 | 35 | 25 | 230 |
| 2.3 | 40 | 25 | 240 |
| 2.4 | 40 | 25 | 250 |
| 2.5 | 40 | 25 | 260 |
| 2.6 | 40 | 30 | 270 |
| 2.8 | 45 | 30 | 290 |
| 3 | 50 | 30 | 310 |
| 3.2 | 50 | 35 | 330 |
| 3.4 | 55 | 35 | 350 |
| 3.6 | 60 | 40 | 370 |
| 3.8 | 60 | 40 | 400 |
| 4 | 65 | 45 | 420 |
| 4.2 | 70 | 45 | 440 |
| 4.4 | 70 | 50 | 460 |
| 4.6 | 75 | 50 | 480 |
| 4.8 | 80 | 50 | 500 |
| 5 | 80 | 55 | 520 |
| 5.2 | 85 | 55 | 540 |
| 5.4 | 90 | 60 | 560 |
| 5.6 | 90 | 60 | 580 |
| 5.8 | 95 | 65 | 600 |
| 6 | 100 | 65 | 620 |
| 6.5 | 105 | 70 | 670 |
| 7 | 115 | 75 | 730 |
| 7.5 | 120 | 80 | 780 |
| 8 | 130 | 90 | 830 |
| 8.5 | 140 | 90 | 880 |
| 9 | 150 | 100 | 940 |
| 9.5 | 150 | 100 | 990 |
| 10 | 160 | 110 | 1050 |
If severe oedema decrease volume by 25% per feed initially and then increase progressively to above volumes.