A09.0
DESCRIPTION
Diarrhoea is a serious common childhood illness evidenced by the passing of frequent profuse loose watery stools. Vomiting may or may not be present.
Diarrhoeal disease is often caused by viral infection but may be due to bacterial infection, dietary or other causes.
Dehydration and metabolic disturbances are common if treatment is not instituted early and may result in severe disease, irreversible organ damage and death in children.
Malnutrition is a serious co-morbidity and/or result of diarrhoeal disease and must be managed correctly, employing ongoing feeding. Feeding, minerals, micronutrients and vitamins are continued except during ileus or shock. See Malnutrition.
In severe malnutrition or in the young infant (< 2 months of age) bacterial co-infection is common.
DIAGNOSTIC CRITERIA
Clinical
The assessment of shock and dehydration in children is not always simple.
A good initial assessment and frequent re-assessments (4-hourly if dehydration is present) are required. In the presence of shock continuous reassessments with appropriate adjustment of care are vital in the care of these children.
Shock is shown by one or more of the following:
Compensated shock:
- delayed capillary refilling time (CRT)
(> 3 seconds), - rapid, weak pulse rate,
- cool peripheries.
Late (Preterminal):
- decreased level of consciousness,
- decreased blood pressure,
- decreased pulse volume.
Dehydration is treated after shock is dealt with:
| Severe dehydration | Some dehydration |
|---|---|
|
Sunken eyes Very slow skin pinch (≥ 2 sec) Drinking poorly |
Sunken eyes Slow skin pinch (< 2 sec) Drinks eagerly Irritable/restless |
Other indicators of dehydration may be sought but do not add substantially to assessment, e.g. depressed fontanelle, absent tears, decreased passage of urine.
Also assess for signs of metabolic, nutritional and other co-morbidities:
- severe malnutrition,
- decreased bowel sounds,
- decreased level of consciousness,
- increased respiratory rate and chest indrawing,
- abnormal tone or floppiness,
- persistent or bile stained vomiting,
- abdominal distension,
- urine for leucocytes or nitrites.
Investigations
- After resuscitation, in children with severe dehydration, shock or other signs of metabolic, nutritional or other co-morbidities:
- sodium, potassium, urea, creatinine, blood acid-base assessment.
- Stool culture if suspected dysentery, typhoid, cholera.
- Urine test strip on fresh/clean urine specimen for leucocytes, nitrites and blood.
- Ascertain HIV status with consent in every child.
GENERAL AND SUPPORTIVE MEASURES
- Adequate initial assessment and frequent re-assessment, including weight, is vital.
- Re-assess the patient continuously while shock persists.
- If dehydration is present, re-assess the patient 4-hourly and immediately correct shock or deterioration.
- Monitor and maintain:
- hydration and circulation,
- normal blood glucose,
- blood pressure,
- blood electrolytes,
- acid-base status.
- Monitor urine output, should be at least 1 mL/kg/hour. This may be difficult in small children with diarrhoea, especially in female infants.
- Monitor body mass regularly. Weigh daily, or 6-hourly if unsure of hydration status and child is very ill or small. This can be used to indicate response of hydration.
- Continue oral feeds during period of diarrhoea:
- if the child is breastfed, continue breastfeeds and encourage the child to feed longer at each feed;
- if the child is exclusively breastfed, give oral rehydration solution (ORS) in addition to each feed;
- if the child is not exclusively breastfed, give ORS and other appropriate feeds, e.g. breast milk substitutes or food based fluids;
- if the child is severely dehydrated or shocked, withhold feeding until stable, usually a few hours only.
MEDICINE TREATMENT
There is no place for antidiarrhoeal medications, i.e. kaolin and pectin, atropine and diphenoxylate, loperamide, or antiemetics in the routine management of acute diarrhoea.
OUTLINE OF PRACTICAL FLUID THERAPY OF DEHYDRATING WATERY DIARRHOEA
With severe malnutrition the assessment of dehydration is more difficult. Avoid intravenous infusions, if possible.
Treatment of dehydration requires more care/more frequent assessments.
1. First treat shock, if present (If no shock, proceed to section 2 below)
If an IV infusion cannot be set up within 5 minutes use an intra-osseus infusion. See Intra-Osseous Infusion in Emergencies . During treatment of shock administer oxygen.
- Sodium chloride 0.9%, IV, 20 mL/kg given as a bolus rapidly.
- After each bolus reassess for persistence of shock, or evidence of circulatory overload.
- Repeat the fluid bolus up to 3 times if shock still persists, provided that evidence of circulatory overload is not present.
- If after the second bolus, i.e. total of 40 mL/kg has been given and the response is inadequate, a third bolus can be started. Move the patient to ICU for CVP monitoring and inotropic support.
Treatment of shock in severe malnutrition
Shock treatment should be more cautious in patients with severe malnutrition due to poor cardiac reserve and high prevalence of gram negative septicaemia.
- Sodium chloride 0.9%, IV, 10 mL/kg administered over 10 minutes.
- Up to 4 boluses may be given. However, deterioration may be due to fluid overload and shock may be due to septicaemia, not always hypovolaemia.
- After 4 boluses (40 mL/kg) further treatment should be in a high care unit.
- Re-assess frequently during treatment of shock. Patient’s response should guide further fluid therapy.
If pulse and respiratory rate increases, increasing liver span and gallop rhythm are found suspect fluid overload/cardiac dysfunction and manage appropriately. See Shock.
When shock has been treated proceed to the management of dehydration.
2. Severe dehydration or some dehydration
2a) If the child has not failed oral rehydration and was not in shock:
- Oral rehydration solution (ORS), oral, 80 mL/kg over 4 hours using frequent small sips (i.e. 5 mL/kg every 15 minutes for 4 hours).
- Give more if the child wants more.
- Show the caregiver how to give ORS with a cup and spoon.
- If child vomits, wait 10 minutes and then continue more slowly.
Nasogastric tube (NGT) rehydration 20 mL/kg/hour over 4 hours can be used as alternative
PLUS
- Encourage caregiver to continue feeding the child, especially breastfeeding.
- Oral feeds should be given at normal volumes and times if:
- the level of consciousness is normal,
- the child is not in severe distress,
- not shocked and,
- has no surgical abdomen.
Review after 4 hours:
- general condition,
- respiratory rate,
- capillary filling time,
- abdomen (liver span),
- level of consciousness,
- if passing urine,
- skin turgor,
- number/quality of stools, and
- sunken eyes.
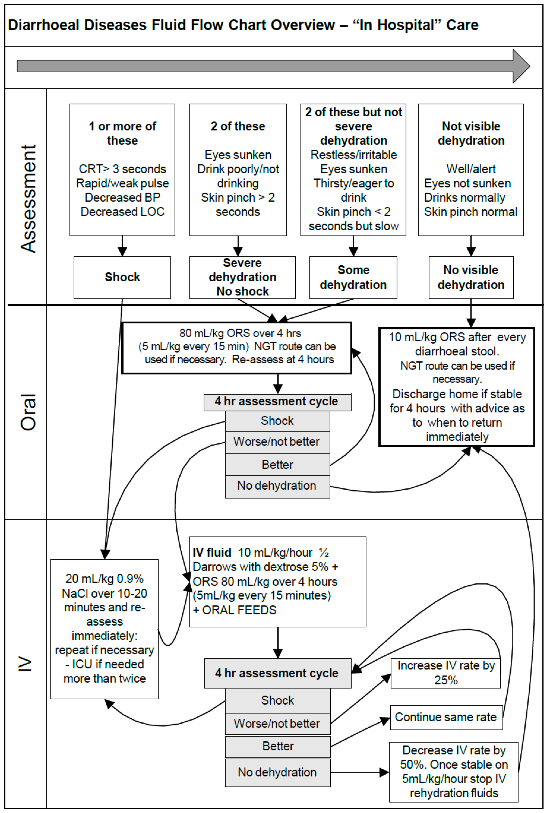
See Figure 1: Summary flow chart for correction of dehydration in diarrhoeal disease.
Assess response 4 hourly.
2b) If child fails the above oral/NGT treatment, was in shock or has already failed at primary health care level then:
IV fluid*
- ½ Darrows/dextrose 5%, IV, 10 mL/kg/hour administered for 4 hours, then re-assess.
* (This rate is in line with current safety evidence but the need for regular reassessment 4-hourly remains.)
PLUS
Oral rehydration solution
- Oral rehydration solution (ORS), oral, 80 mL/kg over 4 hours using frequent small sips (i.e. 5 mL/kg every 15 minutes for 4 hours) or NGT rehydration 20 mL/kg/hour over 4 hours.
PLUS
Oral feeds at normal feed volumes and times if:
- the level of consciousness is normal,
- the child is not in severe distress,
- not shocked and,
- has no surgical abdomen.
Review after 4 hours:
- general condition,
- respiratory rate,
- capillary refilling time,
- abdomen (liver span),
- level of consciousness,
- urine output,
- skin turgor,
- number/quality of stools, and
- sunken eyes.
3. No visible signs of dehydration on presentation or a child stable with no dehydration after treatment of dehydration.
Show the caregiver how to give ORS with a cup and spoon using frequent small sips.
Encourage caregiver to give 10 mL/kg after each diarrhoeal stool until diarrhoea stops.
Instruct the caregiver on how to make and use ORS/SSS at home.
Homemade sugar and salt solution may be used if oral rehydration formula is not available.
HOMEMADE SUGAR AND SALT SOLUTION (SSS)
½ level medicine measure of table salt
plus
8 level medicine measures of sugar
dissolved in 1 litre of boiled (if possible) then cooled water
(1 level medicine measure = approximately 1 level 5 mL teaspoon)
Encourage the caregiver to continue feeding the child, especially breastfeeding.
Instruct the caregiver to give the child extra feeds after the diarrhoea has stopped to make up for the period of inadequate intake.
Child should return to hospital immediately if:
- no improvement,
- blood in stool,
- condition deteriorates,
- fever develops,
- poor drinking or feeding,
- sunken eyes,
- slow skin pinch.
Educate caregivers about hygiene, oral rehydration solution and danger signs of diarrhoea.
Figure 1: Summary flow chart for correction of dehydration in diarrhoeal disease
Metabolic disturbances
Acidosis
Metabolic acidosis will correct with appropriate fluid therapy and does not require additional treatment unless severe, i.e. pH < 7.1, or if the body is unable to correct the deficit, e.g. salicylate poisoning or renal failure.
Additional treatment should only be considered with expert supervision.
Correcting the renal circulation and shock will lead to self-correction in almost all cases.
If correction is necessary: volume of sodium bicarbonate 4.2% required is:
- Sodium bicarbonate 4.2% as a bolus. Dose in mL to be given = 0.3 x base deficit x weight in kg. Review response to assess the need for further correction.
Hypokalaemia
Note: Potassium levels are affected by the degree of acidosis.
If potassium is 2.5 mmol/L to 3.5 mmol/L:
- Potassium chloride, oral, 25–50 mg/kg/dose 8 hourly.
If potassium is < 2.5 mmol/L:
- ½ Darrows/dextrose 5%, 200 mL plus potassium chloride 15%, 2 mL, into the vacoliter:
- 1 mL potassium chloride 15% = 2 mmol potassium. If 2 mL is added in the above solution it gives a combined K+ of 37 mmol/L – do not exceed this amount.
- Mix well before administration.
- Run at normal rehydration rate (as above).
Oral potassium may also be given during this period:
- Potassium chloride, oral, 25–50 mg/kg/dose 8 hourly.
Monitor serum potassium 8–12 hourly. Once above 3.0 mmol/L, stop IV potassium and continue with oral.
Hypernatraemia (> 150 mmol/L)
Severe symptoms usually only develop when the serum sodium is > 160 mmol/L. Symptoms tend to be more severe with acute hypernatraemia (i.e. over a period of hours) while chronic hypernatraemia is often better tolerated because of cerebral compensation.
The true degree of dehydration is often underestimated because the intravascular volume is preserved; signs of intracellular dehydration include lethargy, irritability, "doughy skin", high-pitched cry, hyperreflexia and seizures.
Too rapid reduction of the serum sodium in hypernatraemia can cause cerebral oedema, convulsions and permanent brain injury. More frequent serum sodium monitoring is needed where hypotonic solutions are used.
- Moderate hypernatraemic dehydration (Na 150 - 169 mmol/L):
- If shock is present resuscitate with boluses of 20 mL/kg of 0.9% sodium chloride (see above: step 1 - treat shock).
- Aim to lower the serum sodium slowly with no more than 0.5 mmol/L/hour (10 – 12 mmol/L) over 24 hours.
- Fall of sodium levels more than 1 mmol/L/hour on average means the rehydration rate should be reduced.
- Oral rehydration (10 mL/kg/hour) is preferable to IV rehydration.
- If oral rehydration is tolerated, feeding should be continued.
- Because of longer duration of dehydration, continuous nasogastric tube administration is preferable.
- Fluid is calculated as replacement of deficit (50-70 mL/kg) plus maintenance (over 2 days) over 48 hours.
Calculation of maintenance (mL):
| ≤ 1 year: | 120 mL/kg/24 hours |
| >1 year = sum of the following: | |
| First 10 kg body weight | 100 mL/kg/24 hours |
| Second 10 kg body weight | 50 mL/kg/24 hours |
| Additional weight > 20 kg body weight | 20 mL/kg/24 hours |
If oral/NGT rehydration fails, rehydrate using IV with ½ Darrows dextrose 5% over 48 hours. The sodium concentration of the ½ Darrows can be initially raised to between 90-105 mmol/L by adding 8.4% sodium bicarbonate 15-20 mL to the first 500 mL of ½ Darrows and thereafter, continue with ½ Darrows without any additives.
IV Fluid rate
Rate:
- If 2–10 kg: 6 mL/kg/hour
- If > 10–20 kg: 5 mL/kg/hour
- If > 20–40 kg: 4 mL/kg/hour
- Oral rehydration can be continued for ongoing losses (such as profuse diarrhoea).
- Fluid status, ongoing losses and neurological status should be monitored 2-hourly.
Severe hypernatraemic dehydration (sodium > 170 mmoL (discuss with specialist paediatrician)
This is a medical emergency and referral to and intensive or high care unit should be considered.
- Sodium chloride 0.9%/dextrose 5% plus potassium chloride (see below) is used to correct clinical dehydration for the first 48 hours. Sodium chloride 0.9%/dextrose 5% plus potassium chloride (to 20 mmol/L), IV.
- To every litre 0.9% sodium chloride add 100ml 50% dextrose and 10ml 15% KCl [20mmol potassium]). Infusion rate as above.
- Repeat serum sodium every 8–12 hours to monitor progress.
- Failure to decrease sodium levels usually means the rehydration rate is too slow.
- Frequent clinical reassessment is the key to the safe management of this situation. Serum sodium levels may be done more frequently where this is possible. Adjust the drip rate according to response.
- If convulsions are considered likely, (decreased level of consciousness, hyper-irritable child), in the setting of high serum sodium, consider the use of prophylactic anticonvulsants:
- Phenobarbitone, IV, 20 mg/kg as a single dose.
OR
If IV phenobarbitone not available: - Phenobarbitone, oral, 20–30 mg/kg as a single dose.
- Phenobarbitone, IV, 20 mg/kg as a single dose.
Hyponatraemia
The correction of hyponatraemia is usually only necessary where the serum sodium is significantly decreased (i.e. < 120 mmol/L), or if the patient is symptomatic.
Use sodium chloride 0.9% and add potassium chloride and dextrose as indicated below.
Give at the rate indicated for dehydration and expect correction to have occurred after the following estimated volume:
Volume of sodium chloride 0.9% (mL) = (130–Na+ ) x body weight in kg x 4.
- Administer sodium chloride 0.9%, 200 mL plus potassium chloride 15%, 2 mL plus dextrose 50%, 20 mL into the vacoliter.
- Mix well before administration.
After the calculated volume has been given, resume with:
- ½ Darrows/dextrose 5%, IV, at the required rate.
- Recheck the serum electrolytes.
OR - Oral rehydration solution (ORS), oral, at the required rate.
Antibiotic therapy
Note:
- Antibiotics are not routinely used for diarrhoeal disease.
- During diarrhoea, absorption of antibiotics may be impaired due to intestinal hurry. Give antibiotics orally if administered for intra-luminal effect.
- Other antibiotics for systemic action are best administered parenterally.
- Consider urinary tract infection, or septicaemia in children with severe malnutrition, the immunocompromised and infants < 2 months old.
Dysentery
Treat initially as shigella dysentery:
- Ceftriaxone, IV, 50 mg/kg as a single daily dose for 5 days.
OR - Ciprofloxacin, oral, 15 mg/kg/dose 12 hourly for 3 days.
For entamoeba histolytica (if demonstrated on stool microscopy, or strongly suspected - this is now a relatively uncommon condition in children in South Africa).
- Metronidazole, oral, 15 mg/kg/dose 8 hourly for 7 days.
- Severe disease: treat for 10 days.
Cholera
Treat according to current sensitivities of the organism during epidemic.
See Cholera.
Typhoid
- Ceftriaxone, IV, 50 mg/kg once daily for 10–14 days.
Severe malnutrition
See Malnutrition, severe acute.
- Ampicillin, IV, 50 mg/kg/dose 6 hourly for 5 days.
PLUS - Gentamicin, IV, 6 mg/kg as a single daily dose for 5 days.
- Confirm normal renal function before second dose.
Very young infants < 2 months
- Ampicillin, IV, 25–50 mg/kg/dose 6 hourly for 5 days.
PLUS - Gentamicin, IV, 6 mg/kg as a single daily dose for 5 days.
- Confirm normal renal function before second dose.
Mineral and micronutrient supplementation
All children with diarrhoea.
- Zinc (elemental), oral, for 14 days
- If < 10 kg: 10 mg/day.
- If > 10 kg: 20 mg/day.
- Potassium chloride, oral, 8 hourly.
- If < 6 months: 125 mg.
- If > 6 months: 250 mg.
Do not give if patient is hyperkalaemic or anuric.
REFERRAL
- Inability to correct/treat shock/dehydration.
- Metabolic complications: non-responsive acidosis, severe hypernatraemia (> 170 mmol/l) and symptomatic hypokalaemia.