F40.0-2/F40.8-9/F41.0-3/F41.8-9/F42.0-9 + (F10.0-F19.9/R45.0-8/Z65.0-5/Z65.8-9/Z81.0-4/ Z81.8)
DESCRIPTION
Anxiety is an emotional response to a perceived or anticipated stress. It is diagnosed as a disorder when it is excessive or persistent and impacts daily functioning. Anxiety disorders often present with medically unexplained symptoms such as non-cardiac chest pain, abdominal discomfort and neck and back muscle tension. However, anxiety symptoms may be caused by various medical conditions. In addition, medical conditions are commonly comorbid with anxiety disorders; they may exacerbate the symptoms and the anxiety disorder may worsen the outcome of treatment of the medical condition.
Tobacco, alcohol and other substance use are commonly associated with anxiety disorders. The substance use may be secondary to the disorder or causative or both. If caused by a substance, then an Anxiety Disorder due to the specific substance (F10 – F19) should be diagnosed.
In pregnancy and postnatally, anxiety may impact negatively on the mother’s coping and use of services and is associated with poor psychological and neurodevelopmental outcomes in the child (See PHC STGs and EML, Section Maternal mental health).
- Psychological manifestations of anxiety include panicky feelings, excessive worry, mood changes, irritability, tearfulness, distress, and difficulty concentrating.
- Physical symptoms include muscle tension, headache, abdominal cramps, nausea, palpitations, sweating, a choking feeling, shortness of breath, chest pain, dizziness, numbness, and tingling of the hands and feet.
- People with intellectual disability may present with aggression, agitation, and demanding behaviour instead of anxiety.
- Panic attacks are abrupt surges of intense anxiety with prominent physical symptoms. They may occur in anxiety, mood, and psychotic disorders, and with alcohol and other substance misuse. They are a marker of increased severity of the primary disorder and may indicate a heightened risk of suicide.
- Social phobia (social anxiety disorder) is the fear of social interactions; it usually starts in adolescence. Distorted thoughts are of negative evaluation by others. Self-medication with alcohol or other substances is common and substance intoxication may be the presenting feature.
- Obsessive thoughts and/or compulsive behaviour are a core feature of Obsessive Compulsive Disorder but may also occur in other disorders, particularly tic disorders, autistic spectrum, and psychotic disorders. Themes of the distorted thoughts and compulsions include hygiene (cleaning), security, symmetry, sexual and taboo topics, fears of causing harm, perceived physical defects, hair-pulling or hoarding.
GENERAL MEASURES
Most patients can be treated as outpatients, but some may need to be admitted for diagnostic clarification, containment in extreme distress, or at high risk of suicide.
- Maintain patience and an empathic attitude
- Screen for and manage:
- Causative and comorbid medical illness, e.g. thyroid disease, hyperparathyroidism, phaeochromocytoma, vestibular dysfunctions, epilepsy, and cardiac conditions, hypertension, COPD, asthma, inflammatory bowel disease, GORD.
- Substance misuse, e.g. caffeine, nicotine, alcohol, analgesics, amphetamines and cocaine
- Psychosocial stressors, especially in people with intellectual and other disabilities.
- Psycho-educate the patient and family (with patient’s permission).
- Refer to local support groups. Provide links to self-help literature, web-sites or groups, e.g. www.sadag.org
MEDICINE TREATMENT
Indicated where symptoms are interfering with normal functions of daily living.
Where there is concomitant drug/alcohol dependence or comorbid major depressive episode, an antidepressant may be more appropriate
- Offer a choice of psychotherapy or medication and monitor response.
- Review every 2–4 weeks for 3 months, then 3–6 monthly.
- Partial response: combine medication with psychotherapy.
- If effective, continue for at least 12 months to prevent relapse.
- SSRI, e.g.:
- Fluoxetine, oral.
- Initiate at 20 mg alternate days for 2 weeks.
- Increase to 20 mg daily after 2–4 weeks.
- Delay dosage increase if increased agitation/panicky feelings occur.
- If partial response, increase to 40 mg daily.
OR
If fluoxetine is poorly tolerated:
- Alternative SSRI e.g.:
- Citalopram, oral.
- Initiate at 10 mg daily for the 1st week.
- Then increase to 20 mg daily.
- If partial response, increase to 40 mg daily (not in cardiac disease or >65 years of age).
CAUTION - SSRIs
SSRIs (e.g. fluoxetine, citalopram) may cause agitation initially.
LoEIII [18]
This typically resolves within 2-4 weeks.
Ask about suicidal ideation in all patients, particularly adolescents and young adults (PHC STGs and EML: Suicide risk assessment).
If suicidal ideation present, refer before initiating SSRI.
Once started, monitor closely for clinical worsening, suicidality, or unusual changes in behaviour. Advise families and caregivers of the need for close observation and refer as required.
Note: Continue treatment for a minimum of 12 months. Consider slowly tapering and stopping treatment only if patient has had no/minimal symptoms and has been able to carry out routine daily activities.
Prolong treatment if:
- Previous episode/s of anxiety (extend treatment to at least 3 years).
- Any of: onset in adolescence, severe anxiety, suicidal attempt, sudden onset of symptoms, family history of bipolar disorder (extend treatment to at least 3 years).
- If ≥3 episodes of anxiety (advise lifelong treatment).
For short term use only in severe acute distress:
- Benzodiazepines, e.g.:
- Diazepam, oral, 2.5–5 mg as a single dose.
- Repeat 8 hourly, if required to a maximum of 30 mg daily (in divided doses).
- Half the dose in the elderly or debilitated.
- Duration of therapy: up to 2 weeks, taper off to zero within 6 weeks
- Commence definitive treatment with psychotherapy/SSRI treatment.
CAUTION - BENZODIAZEPINES
- Associated with cognitive impairment – reversible with short-term use and irreversible with long-term use.
- Elderly are at risk of over-sedation, falls and hip fractures.
- Dependence may occur after only a few weeks of treatment.
- Prescribe for as short a period of time as possible.
- Warn patient not to drive or operate machinery when used short-term.
- Avoid use in people at high risk of addiction: e.g. personality disorders and those with previous or other substance misuse.
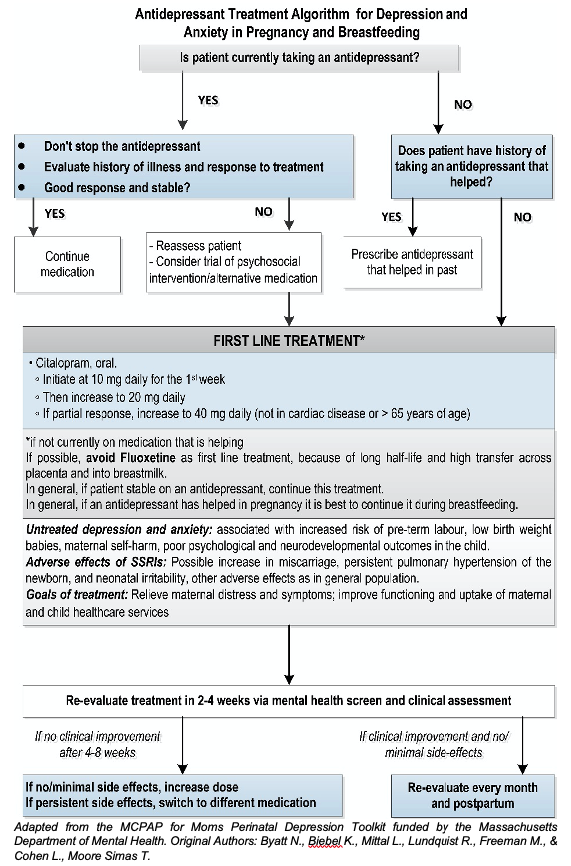
PREGNANCY AND BREASTFEEDING
- SSRI treatment of depression in pregnancy is associated with improved symptoms in the mother and better emotional and psychological development of the child. Benefit is greater with increasing illness severity. Effect of SSRIs on anxiety in pregnancy is less clear.
- Lack of matched case-control studies mean harms of treatment are unclear.
- If stable on an SSRI, do not stop – discuss risk/benefit with mother.
- Index presentations: offer counselling, psychotherapy; discuss risk/benefit of SSRIs.
- Avoid fluoxetine due to long half-life and relatively high concentration in breastmilk. Consider citalopram as alternative
- All antidepressants: possible increased risk of post-partum haemorrhage, transient neonatal symptoms (jitteriness, irritability), and persistent pulmonary hypertension of the newborn.
- Avoid benzodiazepines – some association with neurodevelopmental delay in the child; neonatal sedation if used late in pregnancy.
REFERRAL
- High suicide risk
- Severe symptoms with marked functional impairment
- Co-morbid severe psychiatric or medical conditions
- Poor response to treatment.