F30.0-2/F30.8-9/F31.0-9/F34.0/F34.8-9/F38.0/F39/F06.3 + (F10.0-F19.9/R45.0-8/Z65.0-5/Z65.8-9/Z81.0-4/ Z81.8)
DESCRIPTION
Bipolar disorder (BD) is a heterogenous illness, with high overlap in genetic risk with depression and schizophrenia. Usually follows a chronic, relapsing course, commonly starting in youth. The goal of care is euthymia and optimal functioning according to the person’s ability.
BD may present with:
- an episode of depression, hypomania, mania or mixed mood symptoms
- psychosis
- treatment resistant depression and/or anxiety
- consequences of disturbed behaviour and/or comorbid substance use
- depression in women; men more likely with disruptive behaviour
Diagnostic requirements include, over the lifetime course:
- Bipolar I disorder (BD I): an episode of mania
- Bipolar II disorder (BD II): an episode of hypomania and of depression.
- Other specified BD (BD OS): symptoms of BD plus clinical distress and/or functional impairment but full DSM criteria are not met.
- BD due to another medical condition: direct physiological cause for the bipolar symptoms from another illness, e.g. right-sided cortical or sub-cortical lesions.
In pregnancy and postnatally, bipolar disorder is associated with pre-eclampsia, preterm delivery, and low-birth weight babies. Risk of relapse is high, especially postpartum. Psychotic episodes may be dangerous to mother, baby, or others (See PHC STGs and EML Maternal mental health).
GENERAL MEASURES
Assess and manage in consultation with a psychiatrist.
Risk to self and others is high in BD and unpredictable – repeated risk assessments and a biopsychosocial approach to care is recommended.
Acute management
- Mania, severe depression, and psychosis require urgent hospitalisation in a psychiatric unit, often as an Assisted or Involuntary MHCU.
- Investigate for causative medical conditions, medications, substances.
- Optimise management of comorbid medical illness and substance use.
- Stabilise the immediate mood; electroconvulsive therapy may be required.
- Commence long-term treatment strategy.
- Avoid premature discharge and ensure continuity of care post-discharge.
Long-term management
- Individualise management according to course of illness, cognitive functioning, insight and judgement, and social circumstances.
- Assertive nursing with adherence monitoring is required.
- Screen for and manage comorbid medical illness (thyroid disease, HIV/AIDS, cardiovascular and pulmonary disease, epilepsy, diabetes)
- Screen for and manage substance use.
- Psycho-educate patient, family and carers on the nature of the illness, need for continued treatment, how to self-monitor, early signs of relapse, need for structure and routine.
- Refer to support groups e.g. www.SADAG.org and www.SAFMH.org.za
- Delay important decisions until full recovery from an acute episode; a custodian/ curatorship/ power of attorney may be required.
- Refer to social worker for placement in a residential home, day care or sheltered employment/workshop as needed.
Women in reproductive age-group (See PHC STGs and EMLMaternal mental health).
- Advise family planning – psycho-educate re need to plan pregnancy and comply with antenatal care.
- Manage pregnancy and postpartum period as high-risk for adverse events.
- Select treatment options which are relatively safe in pregnancy.
MEDICINE TREATMENT
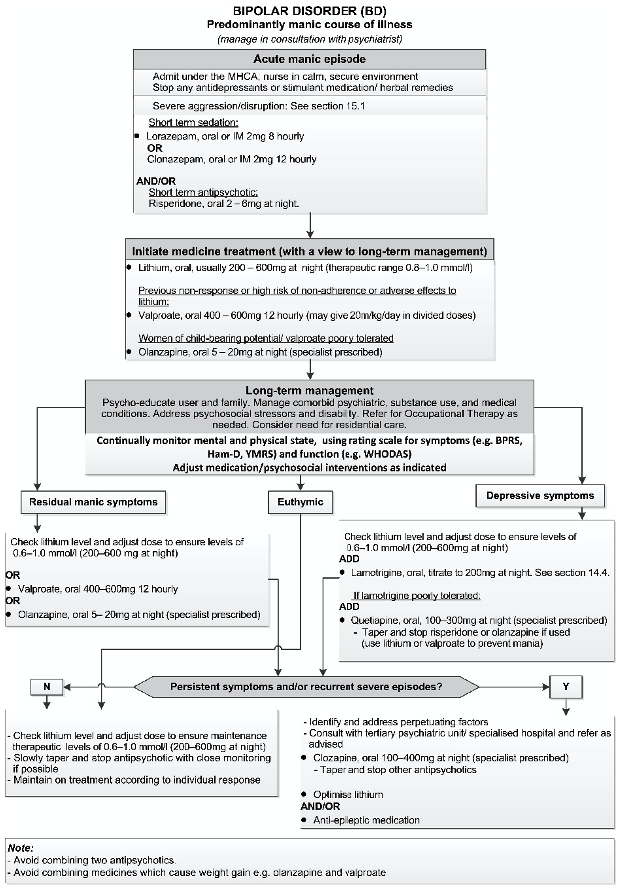
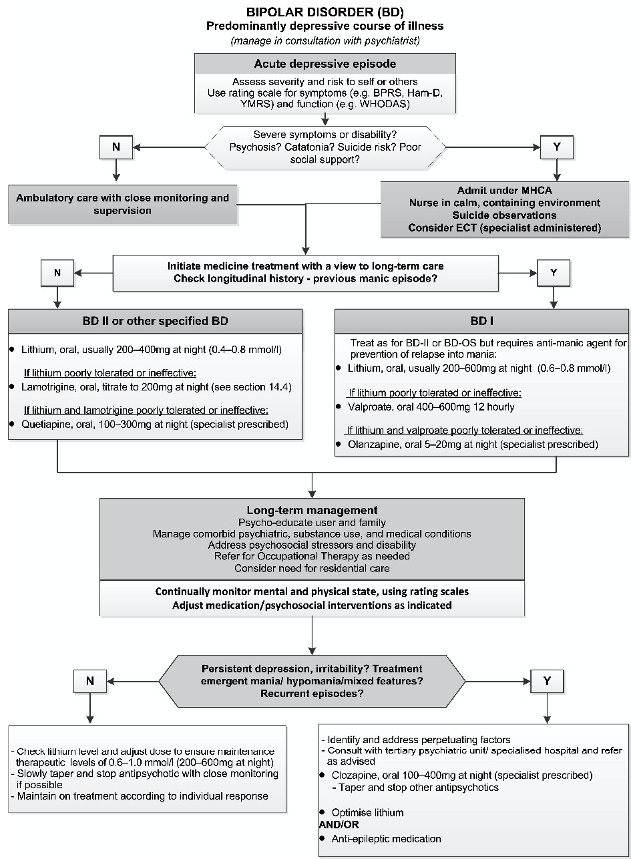
Treatment choice depends on course of illness, gender, comorbid medical, substance use, and psychiatric conditions, and risk of non-adherence. Acute treatment should incorporate a long-term strategy. Combinations of medicines may be required, particularly in depression. See algorithms below.
Lithium is first-line option for long-term treatment:
- Response takes ± 1 week in mania and 6–8 weeks in depression
- Prevents manic episodes by up to 40-50% and depressive episodes by up to 20-30% and reduces aggression, self-harm, and suicide.
- Lithium, oral, usual dose range 200–800 mg at night.
- Pre-treatment: check eGFR, TFTs, calcium, and ECG in patients with cardiovascular risk factors. Proceed if eGFR, ECG normal and any thyroid or parathyroid disease is treated.
- Start with 400 mg (200 mg in elderly or high risk for renal disease).
- Trough (12 hours after night dose) plasma level after 5 days, then 7 days after each dose change, then at 1 month and 3 months.
- Lithium has a narrow therapeutic window. The therapeutic range is 0.8–1.0 mmol/L in acute mania, 0.6–0.8 mmol/l for prevention of mania and 0.4–0.8 mmol/l for prevention of depressive relapse.
- Monitor lithium and eGFR 6-monthly (3-monthly in elderly or medical comorbidity); TSH and calcium annually.
CAUTION - LITHIUM
- Abrupt discontinuation may precipitate mania – taper slowly over 4 weeks.
- Adverse effects include nephrogenic diabetes insipidus, interstitial nephritis, chronic kidney disease; hypothyroidism; hyperparathyroidism; tremor.
- Toxicity occurs with levels >1.2 mmol/l (results in anorexia, nausea, diarrhoea, muscle weakness, drowsiness, ataxia, disorientation, seizures, coma and death. Manage as for lithium poisoning: section 19.9.2.
- Risk of toxicity increased with e.g. change to a low salt diet, dehydration, drug-drug interactions (diuretics, ACE-inhibitors, NSAIDs).
- Therapeutic drug monitoring is essential when using lithium.
- Clinical toxicity may occur even within the therapeutic range.
PREGNANCY AND BREASTFEEDING
Valproate:
- Contraindicated due to high teratogenic risk and adverse neurodevelopmental outcomes with any pregnancy exposure.
- If no alternative, the acknowledgment of risk form must be signed https://www.sahpra.org.za/documents/f150bf3f6.28_Valproate_Annual_Risk_Acknowledgement_Form_Dec18_v1.pdf
- If already on valproate: cross-titrate to an alternative medication if possible (consult specialist if required).
- Not recommended in breastfeeding as associated with adverse neurodevelopmental outcomes.
Lithium:
- 1st trimester exposure associated with increased risk of congenital anomalies.
- Fetal anomaly ultrasound at 18–22 weeks gestation.
- Adjust dose with physiological changes of pregnancy: monitor levels monthly, then weekly after 36 weeks.
- Neonatal complications: goitre, nephrogenic diabetes insipidus, cardiac arrhythmias, cardiac failure, hypotonia, and lethargy.
- Excreted in breast milk, risk to the infant is unknown but toxicity may occur:
breastfeeding is not recommended.
Lamotrigine: Increased hepatic clearance in pregnancy, returns to normal post-partum; adjust dose according to clinical response. May cause a rash in breastfed infant.
Antipsychotics: Considered safest, particularly quetiapine. Increased risk of gestational diabetes and obesity (highest risk with olanzapine, clozapine).
Clozapine is not recommended due to risk of agranulocytosis.
Benzodiazepines: Avoid in pregnancy.
Use only very short-term for severe distress.
- Quetiapine, oral, usual dose range 100–300 mg at night (specialist prescribed).
- Titrate to clinical effect, e.g.: Day 1: 50 mg. Day 2: 100 mg. Day 3: 200 mg. Day 4: 400 mg.
- In the elderly and patients with hepatic impairment: Start with 25 mg and titrate up more slowly according to clinical effect.
BIPOLAR DISORDER
REFERRAL
All patients to be managed in consultation with a psychiatrist, refer as advised, particularly if:
- High risk to self or others at any time.
- Rapid cycling (repeated episodes despite treatment).
- Poor response to treatment with persistent depressive, manic, or mixed symptoms.