N18.1-5/N18.9
- Description
- Treatment and prevention strategies according to stages
- General measures
- Medicine treatment
- Consult with a specialist at the local referral centre
- Referral
DESCRIPTION
Structural or functional kidney damage present for >3 months, with or without a decreased estimated glomerular filtration rate (eGFR).
Markers of kidney damage include:
- proteinuria; ACR-urine (albumin creatinine ratio) ≥30 mg/g or ≥3 mg/mmol; PCR-urine (protein creatinine ratio) >0.05 g/mmol
- urine dipstick positive for blood and/or protein (for females with haematuria: exclude current menstrual cycle)
- increased serum creatinine or low eGFR
- abnormal kidneys on ultrasound, e.g. polycystic, small in size, scarring
- abnormalities on renal biopsy
- electrolyte abnormalities due to tubular disorders
- history of kidney transplant
eGFR calculator online access: https://www.kidney.org/apps/professionals/egfr-calculator
Common causes of CKD include:
| Category | Example |
| Vascular | Hypertension, vasculitis etc. |
| Glomerular diseases |
Diabetes, autoimmune diseases, systemic infections, drugs, neoplasia |
| Tubulointerstitial diseases |
UTI, drug induced interstitial nephritis (e.g. rifampicin, allopurinol, fluoroquinolones, sulphonamides) |
| Structural |
Polycystic kidney/s, renal artery stenosis, small or enlarged kidneys, renal masses, obstruction (stones, strictures) |
| Others | Congenital |
Chronic kidney disease can be entirely asymptomatic
until over 75% of kidney function is lost.
TREATMENT AND PREVENTION STRATEGIES ACCORDING TO STAGES
Adverse outcomes of CKD can often be prevented or delayed through early detection and treatment of risk factors for CKD.
In patients with CKD, the stage of disease should be assigned based on the level of kidney function according to the classification below, irrespective of diagnosis.
Adults with early CKD i.e. stages 0–3 can all be managed at primary care level once the cause and plan for care has been established.
All stage 4 and 5 patients require referral/consultation with a specialist. If the patient is a candidate for long-term dialysis nephrological referral is advised.
Prognosis of CKD by GFR and albuminuria categories: KDIGO 2012
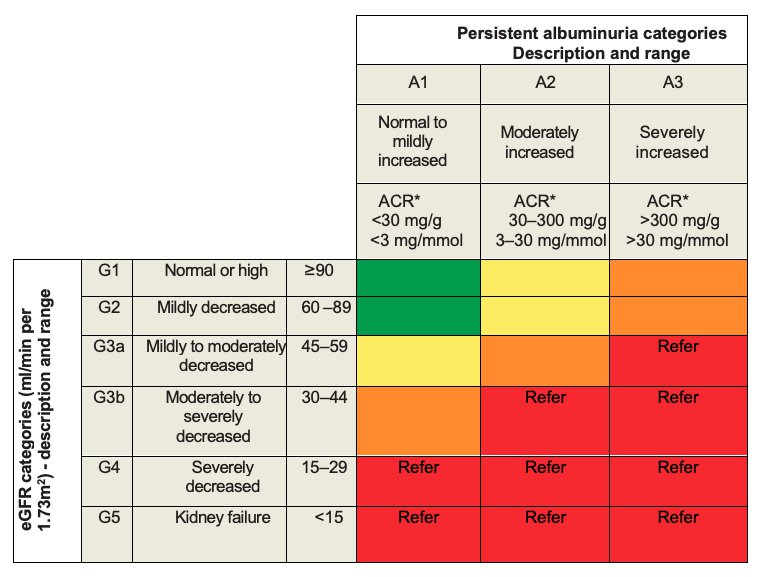
ACR: albumin to creatinine ratio in urine specimen.
Green: low risk (if no other markers of kidney disease, no CKD); yellow: moderately increased risk; orange: high risk; red: very high risk; A1, A2, A3 = categories of albuminuria; G1, G2, G3a, G3b, G4, G5 = categories of eGFR
Adapted from: Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014 Jan;85(1):49-61. https://www.ncbi.nlm.nih.gov/pubmed/24284513
GENERAL MEASURES
- Address cardiovascular disease risk factors. See Ischaemic heart disease and atherosclerosis, prevention.
- Limit salt intake unless salt wasting kidney disease.
- Limit dietary protein intake to 0.8 g/kg/day.
- Avoid nephrotoxic medicines like NSAIDs.
- Regular exercise, target BMI according to South African calculations.
- Screen for proteinuria.
- If urine dipstick 1+ or greater, repeat on a properly collected midstream urine specimen on another occasion.
- If proteinuria persists, quantify protein with a spot urine protein creatinine ratio. Significant proteinuria = spot urine PCR of >0.1 g/mmol.
- If urine dipstick < 1+, ACR.
Patients differ in their ability to excrete a salt and water load and therefore fluid balance should be individualised.
MEDICINE TREATMENT
The following interventions may delay progression of renal disease.
Proteinuria reduction
Ideal targets are: PCR <0.03 g/mmol or ACR <3 mg/mmol.
Most benefit is achieved by reducing protein creatinine ratio to <0.1 g/mmol or ACR <100 mg/mmol.
- Start treatment with a low dose of ACE-inhibitor and titrate up to the maximum tolerated dose, e.g.
- Enalapril, oral.
- Start with 5 mg 12 hourly and titrate to 20 mg 12 hourly, if tolerated.
- Monitor creatinine and potassium after 2 weeks if eGFR <60 mL/minute and after 4 weeks if eGFR >60 mL/minute.
- If creatinine increases by >20% from the baseline, stop ACE-inhibitor and consult a specialist.
ACE-inhibitor not tolerated due to intractable cough (specialist initiated):
- Consider an angiotensin II receptor blocker (ARB), e.g.:
- Losartan, oral,
- Start with 50 mg daily and titrate to 100 mg daily, if tolerated.
- Replacing ACE-inhibitor with ARB does not preclude the risk of angioedema.
CAUTION
ACE-inhibitors and ARBs can cause or exacerbate hyperkalaemia in CKD. Check the serum potassium before starting these medicines, and monitor serum potassium on therapy.
Hypertension
Optimise BP control with additional antihypertensive agents. BP control results in a lowering of proteinuria and slower decline in eGFR.
Target BP for patients with hypertension: < 140/90 mmHg.
Target BP for patients with hypertension and confirmed CKD and/or diabetes: <130/80 mmHg.
See: Hypertension.
Hyperlipidaemia
If hyperlipidaemia is a co-existent cardiovascular risk factor, manage according to Ischaemic heart disease and atherosclerosis, prevention.
Diabetes mellitus
In diabetics, optimise control according to Diabetes mellitus.
In diabetics with kidney disease there is an increased risk of hypoglycaemia.
Insulin is the safer option to control blood glucose in patients with eGFR<60 mL/minute.
Note:
- Insulin requirements will decrease as renal disease progresses.
- Stop glibenclamide when eGFR <60 mL/minute because of an increased risk of hypoglycaemia.
- Reduce metformin dose when eGFR <60 mL/minute (maximum dose 500 mg 12 hourly).
- Discontinue metformin when eGFR <30 mL/minute because of the risk of lactic acidosis.
Fluid overload and oedema
- Furosemide, oral, 40 mg 12 hourly.
When fluid overloaded and eGFR <60 mL/minute, start:
- Furosemide, oral, 40 mg 12 hourly.
- Titrate to a maximum of 500 mg 12 hourly.
- Furosemide is ineffective when patients are on dialysis and anuric.
Hypocalcaemia and hyperphosphataemia
The aim is to lower phosphate levels and maintain normal calcium levels to ensure calcium phosphate product (i.e. Ca x PO4) < 4.4 mmol2/L2, to prevent calcium deposition in vessels and tissue which aggravates vascular disease.
Restrict dietary phosphate intake. (Dietitian consultation)
http://kidneyfoundation.cachefly.net/professionals/KDOQI/guidelines_bone/guide4.htm
Patients with CKD stage 3–5, not on dialysis:
Hyperphosphataemia and/or hypocalcaemia:
- Calcium carbonate, oral, equivalent to elemental calcium, approximately 500 mg 8 hourly with meals.
- Increase to approximately 1 g 8 hourly with meals, if hyperphosphatemia persists.
Hypocalcaemia and low or normal serum phosphate:
- Calcium carbonate, oral, equivalent to elemental calcium, approximately 500 mg 8 hourly between meals, increase to approximately 1 g 8 hourly between meals.
In patients with CKD stage 5 who are not candidates for renal replacement therapy, the benefits of phosphate binding are unclear, and regular PTH (parathyroid hormone) monitoring is not necessary.
Patients considered suitable candidates for renal replacement therapy:
Monitor Ca++, PO4 and PTH levels, as per table: Staging of kidney disease.
For hyperphosphataemia uncontrolled on calcium carbonate:
- Aluminium hydroxide BP (300 mg/5 mL), oral, 10 mL 8 hourly. Specialist initiated.
- To prevent dementia-associated aluminium toxicity, do not use for longer than 3 months.
For hyperparathyroidism, initiate when PTH levels >2 times upper limit of normal range: (Specialist initiated)
(N25.8)
- Calciferol, oral, 50 000 IU once weekly.
OR
- Calcitriol, oral, 0.25–4 mcg daily.
Anaemia associated with CKD in patients on dialysis programmes N18.1-5†/N18.9† + (D63.8*/Z49.1-2)
Patients on chronic haemodialysis or peritoneal dialysis are often anaemic due to iron deficiency and deficiency of erythropoietin (EPO).
Simultaneous administration of iron and EPO is recommend, as EPO should be administered in a patient with normal iron stores. Adequate iron stores are required to assist with red blood cell production immediately after EPO administration (see: Anaemia, iron deficiency).
- Iron, elemental, oral. See Anaemia, iron deficiency.
- If no response, consider parenteral iron.
AND
- Erythropoietin, 40–50 IU/kg/dose, IV/SC 2–3 times weekly and assessed at 4 weekly intervals.
- Administer IV dose over 1–5 minutes.
- If necessary, dose may be increased by 25 IU/kg.
- Note: There is an increased risk of cardiovascular events with haemoglobin levels >12 g/dL.
Definitive treatment, e.g. transplantation, usually improves anaemia. It is important to identify factors likely to aggravate anaemia, e.g. iron deficiency and infection.
Acidosis and hyperkalaemia
Specialist consultation for possible renal replacement therapy.
Check all medicines for possible dose adjustments. http://www.globalrph.com/index_renal.htm
CONSULT WITH A SPECIALIST AT THE LOCAL REFERRAL CENTRE
- Unknown cause of kidney failure.
- Rapid deterioration in renal function.
- Resistant hypertension despite appropriate medication and adherence.
- All patients with persistent proteinuria: on urine dipstick ≥ 1+ or proteinuria >1 g/24 hours (PCR >0.1 g/mmol).
REFERRAL
- All ESRD patients who may qualify for long term dialysis programs. See : Renal replacement therapy.
- CKD stage 3 and above (see prognosis table).