S61.0 + (W46.22 + Z20.6 + Z29.8)
DESCRIPTION
Antiretroviral therapy may prevent the risk of acquiring HIV following a significant occupational exposure.
It is essential to document occupational exposures adequately for possible subsequent compensation.
Other blood borne infections (hepatitis B and C) should also be tested for in the source patient and appropriate prophylaxis instituted in the case of hepatitis B.
Assessing the risk of occupational exposures
The risk of acquiring HIV following occupational exposure is determined by the nature of the exposure and the infectiousness of the source patient. High-risk exposures involve exposure to a larger quantity of viruses from the source patient, either due to exposure to larger quantity of blood or because the amount of virus in the blood is high.
Any one of the following associated with an increased risk of HIV transmission:
- deep percutaneous sharps injuries
- percutaneous exposure involving a hollow needle that was used in a vein or artery
- visible blood on the sharp instrument involved in a percutaneous injury
- the source patient has terminal AIDS or is known to have a high viral load, i.e. >100 000 copies/mL
In instances when the risk of infection is extremely low or non-existent, post-exposure prophylaxis (PEP) is not indicated, as the risks of PEP will far outweigh the benefits. PEP is NOT indicated when:
- The material the healthcare worker was exposed to is not infectious for HIV in the occupational setting, e.g. vomitus, urine, faeces or saliva, unless these are visibly blood stained.
- The exposure was on intact skin.
- The source patient is HIV negative, unless there are clinical features to suggest seroconversion illness, in which case PEP should be commenced until further tests are done – consult with a virologist or infectious diseases specialist.
- The healthcare worker is HIV infected, as this person should be assessed for ART initiation.
PEP REGIMENS
PEP should be commenced as soon as possible after the injury. Do not delay initiating PEP while awaiting confirmatory test results on the source patient and health care worker. PEP should be considered up to 72 hours after exposure and, in exceptional circumstances involving high-risk exposures, PEP may be considered up to 7 days after exposure.
When PEP is indicated:
- Tenofovir, oral, 300 mg daily for 4 weeks (provided baseline eGFR is >50 mL/minute).
and
- Lamivudine, oral, 200 mg daily for 4 weeks
and
- Dolutegravir, oral 50 mg once daily for 4 weeks.
In WOCP, pregnant women <6 weeks gestation, or where DTG is not tolerated:
- Tenofovir, oral, 300 mg daily for 4 weeks (provided baseline eGFR is >50 mL/minute).
and
- Emtricitabine, oral, 200 mg daily for 4 weeks.
and
- Atazanavir/ritonavir 300/100 mg daily for 4 weeks.
Or
- Lopinavir/ritonavir 200/50 mg, oral, 2 tablets 12 hourly for 4 weeks.
If tenofovir is contraindicated or if source patient is known to be failing a tenofovir based regimen, replace tenofovir and emtricitabine with:
- Zidovudine, oral, 300 mg 12 hourly for 4 weeks.
and
- Lamivudine, oral, 150 mg 12 hourly for 4 weeks.
PEP is generally not well tolerated. Adverse effects occur in about half of cases and therapy is discontinued in about a third. Efavirenz is not recommended as it is very poorly tolerated in PEP.
Zidovudine often causes nausea and headache. If zidovudine is not tolerated, switch to tenofovir (check baseline eGFR as above).
Lopinavir/ritonavir often causes diarrhoea. If lopinavir/ritonavir is not tolerated switch to atazanavir/ritonavir. Atazanavir/ritonavir often causes unconjugated jaundice, which is benign but may not be tolerated, in which case switch to lopinavir/ritonavir.
Recommendations for post exposure prophylaxis (PEP) after occupational exposure to infectious material (includes blood, CSF, semen, vaginal secretions and synovial/pleural/ pericardial/ peritoneal/amniotic fluid) from HIV seropositive patients are given in the table, below.
PEP for healthcare worker following occupational HIV exposure:
| Exposure | HIV Status of source patient | |
| Negative | Unknown or Positive | |
| Intact skin | no PEP | no PEP |
|
Mucosal splash or non-intact skin or percutaneous injury |
no PEP | 3-drug regimen (PI-based) |
When the source patient is known to be failing ART, modify the PEP regimen:
- If the patient is on zidovudine , use tenofovir.
- If the patient is on tenofovir then use zidovudine.
Patients failing 2nd line ART usually have no resistance to protease inhibitors, so lopinavir/ritonavir should still be effective, but consultation with a virologist or infectious diseases physician is recommended for advice on which ARVs to use for PEP in this setting.
PEP for healthcare workers following hepatitis B exposure
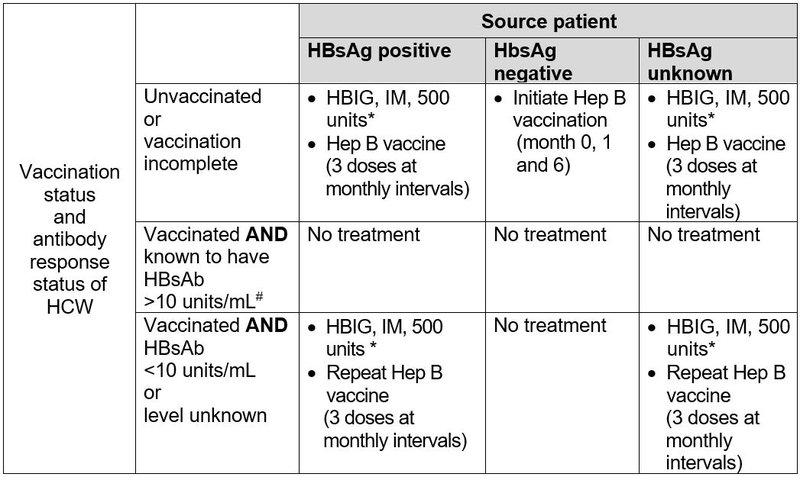
* HBIG and first dose of vaccine to be given simultaneously, but at different sites.
# If the delay in obtaining HBsAb results is more than 24 hours initiate treatment as for vaccinated AND HBsAb < 10 units/mL.
After vaccination ensure the health care worker has a HBsAb > 10 units/mL 1 – 2 months after the last vaccine dose.
| Source patient | Exposed health care worker | Exposed health care worker | Exposed health care worker | Exposed health care worker | |
| Baseline | Baseline | 2 weeks | 6 weeks | 4 months | |
| HIV |
Rapid test PLUS ELISA |
Rapid test PLUS ELISA |
ELISA | ELISA | |
| Hepatitis B | Surface antigen | Surface antibody* | |||
| Hepatitis C | HCV antibody | HCV antibody* | HCV PCR* | ||
| Syphilis | RPR/ TP antibody | RPR/TP antibody* | RPR/TP antibody* | ||
| Creatinine | If TDF part of PEP | If TDF part of PEP | |||
| FBC | If AZT part of PEP | If AZT part of PEP | |||
*Only if source patient was positive.