T30.0-3 + (T31.0-9/Y34.99
DESCRIPTION
Skin and tissue damage caused by:
- exposure to extremes of temperature,
- contact with an electrical current,
- exposure to a chemical agent, and
- radiation.
ASSESSMENT OF BURNS
|
Depth of burn wound |
Surface /colour |
Pain sensation/healing |
|---|---|---|
|
Superficial or epidermal |
Dry, minor blisters, erythema |
|
|
Partial thickness superficial or superficial dermal |
Blisters, moist |
|
|
Partial thickness deep or deep dermal |
Moist white or yellow slough, red mottled |
Generally needs surgical debridement and skin graft |
|
Full thickness (complete loss of skin) |
Dry, charred whitish, brown or black |
|
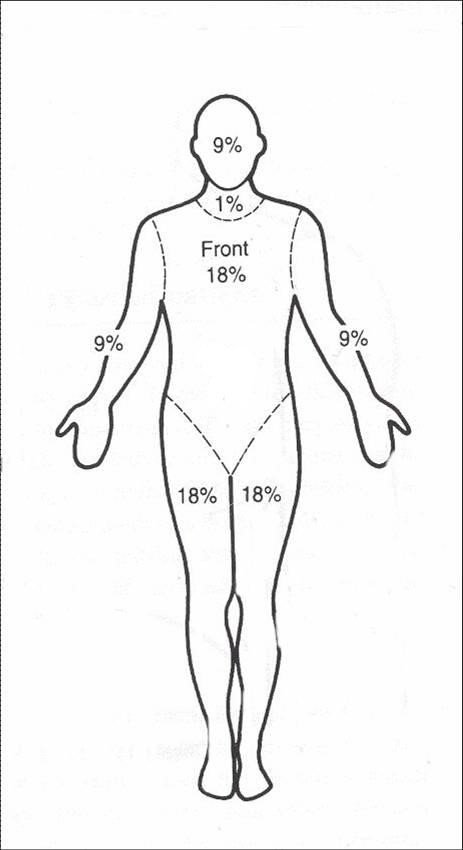
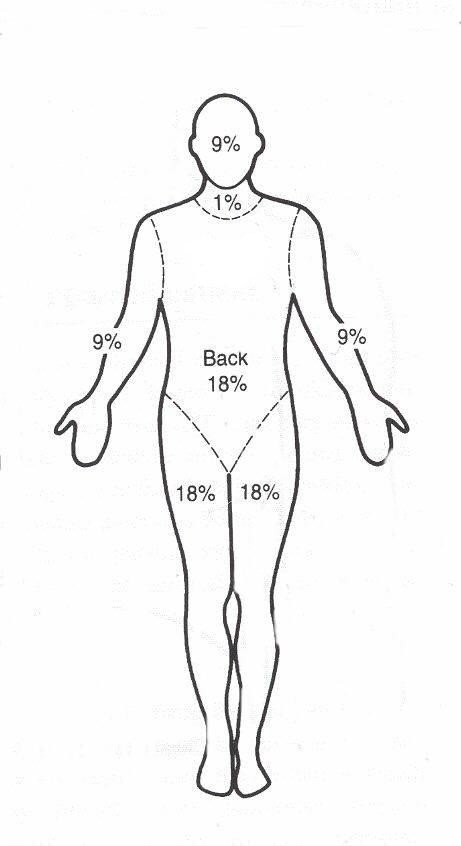
The figures below are used to calculate body surface area %.
These diagrams indicate percentages for the whole leg/arm/head (and neck in adults) not just the front or back.
Children ≥8 years and adults
Source: Karpelowsky JS, Wallis L, Madaree A, Rode H; South African Burn Society. South African Burn Society burn stabilisation protocol. S Afr Med J. 2007 Aug;97(8):574-7. http://www.ncbi.nlm.nih.gov/pubmed/17966146
GENERAL MEASURES
- Assess airway, breathing
- Look for signs of inhalational burn- history of hot gas, smoke, steam.
- INTUBATE if significant airway obstruction present or WORSENING symptoms.
- Intubation is necessary in the case of unconscious patients, hypoxic patients with severe smoke inhalation, or patients with flame or flash burns involving the face and neck if there is evidence of compromised airway patency.
- Intubate early if burns are inhalational, or in the presence of pharyngeal burns with soft tissue swelling, as these patients frequently tend to develop respiratory failure.
- Close monitoring is essential during the first 24-48 hours
- If breathing is compromised because of tight circumferential trunk burns, consult with burn centre surgeons immediately. Urgent escharotomies may be required to facilitate chest expansion
- Assess circulation
- Establish large-bore intravenous (IV) lines and provide resuscitation bolus fluid.
- Reminder: IV lines may be placed through the burned area if necessary (suture to secure).
- Assess neurological state of the patient
- Assess for associated trauma related injuries
- Secure the C–spine with an inline stabilising collar, when the mechanism of injury could indicate additional trauma.
- Identify potential sources of internal bleeding.
- Stop any external bleeding.
- Remove any sources of heat or chemicals. Removal constrictive clothing/accessories.
- Estimate percentage of total body surface area involved.
- Support vital organ function.
- Look for aggravating comorbidities, e.g. seizures, hyperkalaemia, renal failure.
- Assess need for decompression incisions: escharotomies
- Local wound care: Clean superficial burns can be managed by occlusive dressings. Deeper wounds may have to be excised and grafted.
- Rehabilitation involving physiotherapy and occupational therapy.
Burn injuries put patients into a hypermetabolic state which requires early and adequate nutritional support. Seek early guidance from local burns centre. See Nutritional support.
MEDICINE TREATMENT
Fluid replacement
Burns ≤ 10% Total Body Surface Area (TBSA):
- Oral rehydration solution.
Burns >10% of TBSA:
- Sodium chloride 0.9%, IV fluid for resuscitation, replacement and maintenance.
Calculation of fluid replacement
Replacement fluids for burns
- First 24 hours:
- Sodium chloride 0.9%, IV.
- Calculate total fluid requirement in 24 hours: Total % burn x weight (kg) x 4 mL.
- Give half this volume in the 1st 8 hours.
- Administer remaining fluid volume in next 16 hours.
Note: If urine output is not adequate, increase fluids for the next hour by 50%. Continue at a higher rate until urine output is adequate, then resume normal calculated rate. Aim for urine output 0.5 mL/kg/hr.
Analgesia
Ensure adequate analgesia particularly at change of dressing, i.e.:
- Morphine, IV, to a total maximum dose of 10 mg (See Appendix II, for individual dosing and monitoring for response and toxicity).
AND
- Paracetamol, oral, 1 g 4–6 hourly when required.
- Maximum dose: 15 mg/kg/dose.
- Maximum daily dose: 4 g in 24 hours.
Tetanus prophylaxis Z23.5
Tetanus toxoid vaccine, IM, 0.5 mL immediately.
Local Wound Care
- Melted plastic and tar can be removed with the topical application of liquid paraffin solution
- Wash burn wounds with soap and water or 1% chlorhexidine.
- Cool burns less than 3 hours old with cold tap water for at least 30 minutes and then dry the patient.
- Keep the wound clean and dress with sterile dressings.
For chemical burns
- Remove all clothing.
- Brush powdered chemicals off the wound
- Flush chemical burns for a minimum of 30 minutes using copious volumes of running water.
- Reminder: Never neutralise an acid with a base or vice versa.
- Determine what chemical (and what concentration) caused the injury.
- Ocular burns: T26.4 + (Y34.99)
- Sodium chloride 0.9% gentle eye washes or irrigations as soon as possible. Follow with an ophthalmology consultation
For electrical burns
- Differentiate between low-voltage (<1 000 v) and high-voltage (>1 000 v) injuries.
- Attach a cardiac monitor; treat life-threatening dysrhythmias as needed.
- Suspect compartmental syndrome, consider escharotomies.
Stress ulcer prophylaxis
Feeding patients provides protection against gastric ulcer developing and prophylaxis is not necessary in patients who are tolerating feeds.
Note: Pharmacokinetic parameters are altered in patients with severe burns, notably an increased volume of distribution. An appropriate loading dose should be given of certain medicines, e.g. aminoglycosides. Therapeutic drug monitoring (TDM) may inform dosing and should be requested, if available.
Discuss the following cases with a burns specialist:
- Burns >15% body surface area (BSA) or >10% BSA >50 years of age.
- Burns of face, hands, feet, genitalia, perineum or involving joints.
- Electrical burns, including lightning burns.
- Chemical burns.
- Inhalation injury or burns.
- Burns associated with major trauma.
- Circumferential burns.